Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3B - Obesity / Biliary-Pancreas
54 - Identifying Diagnostic Patterns for Exocrine Pancreatic Insufficiency in Adults With Chronic or Recurrent Acute Pancreatitis: Findings From the PACT-CP Registry
Tuesday, October 29, 2024
3:35 PM - 3:45 PM ET
Location: Terrace Ballroom 2-3
.jpg)
Jodie A. Barkin, MD, FACG
Associate Professor of Clinical Medicine
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Rahul Pannala, MD1, Paramjit Benipal, MD2, Kenneth L. Buch, MD3, David C.. Whitcomb, MD, PhD4, Jennifer Pack, MSN5, Janine Twal, PharmD5, Jodie A. Barkin, MD, FACG6
1Mayo Clinic, Scottsdale, AZ; 2Marian Regional Medical Center; Santa Maria Gastroenterology Medical Group, Santa Maria, CA; 3Genesis, Encino, CA; 4University of Pittsburgh, UPMC and Ariel Precision Medicine, Pittsburgh, PA; 5Nestlé Health Science, Bridgewater, NJ; 6University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: Lack of standard diagnostic criteria and widely available, accurate, and feasible testing may contribute to the underrecognition/undertreatment of exocrine pancreatic insufficiency (EPI). We evaluate patterns in EPI diagnosis using a real-world, prospective PAtient-CenTric Chronic Pancreatitis (PACT-CP) registry of patients with recurrent acute pancreatitis (RAP) or chronic pancreatitis (CP) and EPI.
Methods: This US-based longitudinal, noninterventional study (NCT05762445) follows participants up to 5 years. Eligible adults are those diagnosed with RAP/CP, have suspected/confirmed EPI by an expert healthcare practitioner, and are receiving pancreatic enzyme replacement therapy (PERT) at enrollment. Data were analyzed descriptively. For this analysis, the dates of symptom onset vs EPI diagnosis were truncated at the year (eg, 05/15/2024 to 2024) to accommodate for an unknown month or day.
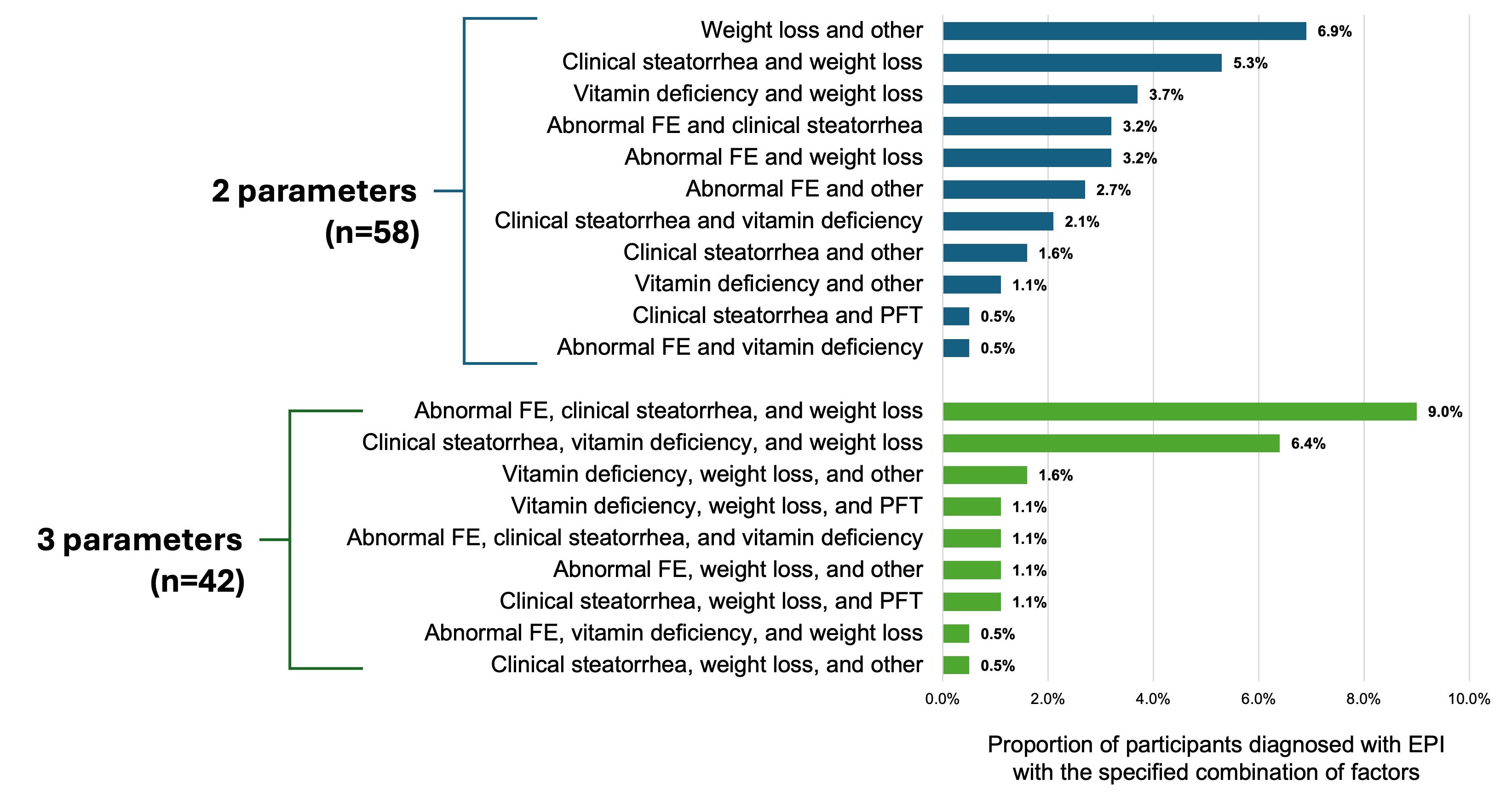
Results: As of May 20, 2024, 200 participants were enrolled in the registry. Mean (SD) age was 60.2 (13.8) years (n=186); 50.0% were men and 83.9% were White. As of April 19, 2024, for participants who received an EPI diagnosis after symptom onset (n=179), average time to diagnosis of suspected/confirmed EPI was 3 years and the majority (55.9%) were diagnosed within 1 year. There were 20 (11.2%) participants who received an EPI diagnosis beyond 5 years after symptom onset. The most common forms of evidence of suspected/confirmed EPI diagnosis (n=188) were weight loss (55.9%), clinical steatorrhea (41.0%), and abnormal fecal elastase-1 test (33.0%). “Other” parameter was used in 26.6% of participants and included nausea, vomiting, and imaging findings. Clinicians reported using 1 symptom/clinical test to diagnose EPI in 34.1%, 2 parameters in 32.4%, 3 parameters in 23.5%, and 4 parameters in 6.7% of participants. The most common combinations of 2 or 3 clinical symptoms/tests as criteria to diagnose EPI were abnormal fecal elastase-1 test, clinical steatorrhea, and weight loss (9.0%); weight loss and “other” symptom/test (6.9%); and clinical steatorrhea, vitamin deficiency, and weight loss (6.4%; Figure).
Discussion: A lag between symptom onset and EPI diagnosis for participants in the PACT-CP registry was observed, as expected and in line with the published literature. Patients with RAP/CP and EPI are diagnosed with a variety of clinical factors and improved objective measures are needed to accurately and appropriately diagnose EPI for timely initiation of PERT.
Disclosures:
Rahul Pannala, MD1, Paramjit Benipal, MD2, Kenneth L. Buch, MD3, David C.. Whitcomb, MD, PhD4, Jennifer Pack, MSN5, Janine Twal, PharmD5, Jodie A. Barkin, MD, FACG6, 54, Identifying Diagnostic Patterns for Exocrine Pancreatic Insufficiency in Adults With Chronic or Recurrent Acute Pancreatitis: Findings From the PACT-CP Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Scottsdale, AZ; 2Marian Regional Medical Center; Santa Maria Gastroenterology Medical Group, Santa Maria, CA; 3Genesis, Encino, CA; 4University of Pittsburgh, UPMC and Ariel Precision Medicine, Pittsburgh, PA; 5Nestlé Health Science, Bridgewater, NJ; 6University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: Lack of standard diagnostic criteria and widely available, accurate, and feasible testing may contribute to the underrecognition/undertreatment of exocrine pancreatic insufficiency (EPI). We evaluate patterns in EPI diagnosis using a real-world, prospective PAtient-CenTric Chronic Pancreatitis (PACT-CP) registry of patients with recurrent acute pancreatitis (RAP) or chronic pancreatitis (CP) and EPI.
Methods: This US-based longitudinal, noninterventional study (NCT05762445) follows participants up to 5 years. Eligible adults are those diagnosed with RAP/CP, have suspected/confirmed EPI by an expert healthcare practitioner, and are receiving pancreatic enzyme replacement therapy (PERT) at enrollment. Data were analyzed descriptively. For this analysis, the dates of symptom onset vs EPI diagnosis were truncated at the year (eg, 05/15/2024 to 2024) to accommodate for an unknown month or day.
Results: As of May 20, 2024, 200 participants were enrolled in the registry. Mean (SD) age was 60.2 (13.8) years (n=186); 50.0% were men and 83.9% were White. As of April 19, 2024, for participants who received an EPI diagnosis after symptom onset (n=179), average time to diagnosis of suspected/confirmed EPI was 3 years and the majority (55.9%) were diagnosed within 1 year. There were 20 (11.2%) participants who received an EPI diagnosis beyond 5 years after symptom onset. The most common forms of evidence of suspected/confirmed EPI diagnosis (n=188) were weight loss (55.9%), clinical steatorrhea (41.0%), and abnormal fecal elastase-1 test (33.0%). “Other” parameter was used in 26.6% of participants and included nausea, vomiting, and imaging findings. Clinicians reported using 1 symptom/clinical test to diagnose EPI in 34.1%, 2 parameters in 32.4%, 3 parameters in 23.5%, and 4 parameters in 6.7% of participants. The most common combinations of 2 or 3 clinical symptoms/tests as criteria to diagnose EPI were abnormal fecal elastase-1 test, clinical steatorrhea, and weight loss (9.0%); weight loss and “other” symptom/test (6.9%); and clinical steatorrhea, vitamin deficiency, and weight loss (6.4%; Figure).
Discussion: A lag between symptom onset and EPI diagnosis for participants in the PACT-CP registry was observed, as expected and in line with the published literature. Patients with RAP/CP and EPI are diagnosed with a variety of clinical factors and improved objective measures are needed to accurately and appropriately diagnose EPI for timely initiation of PERT.
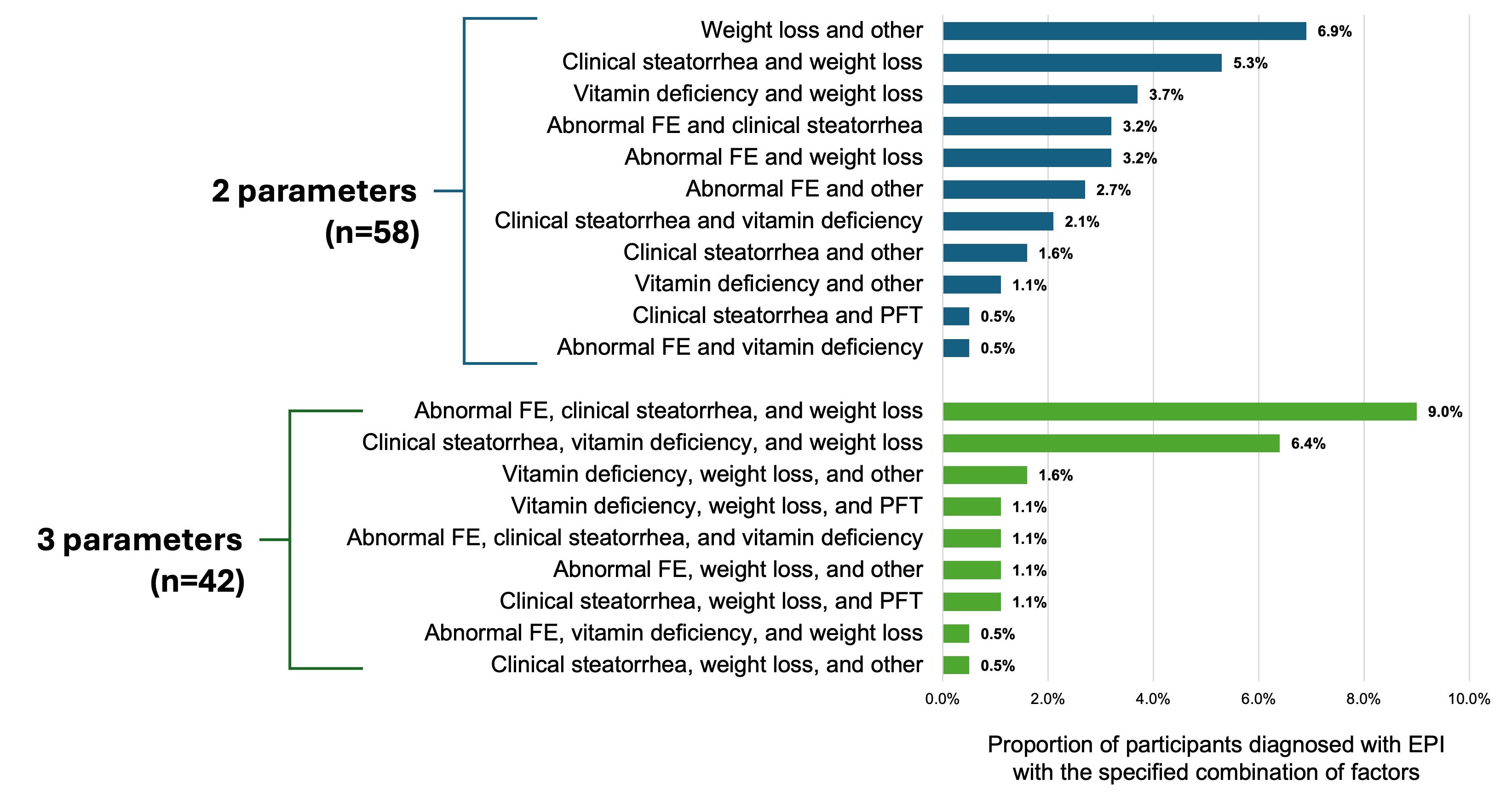
Figure: Combinations of clinical symptoms and testing methods used as evidence for suspected/confirmed EPI diagnosis
All other combinations of the clinical symptoms/testing (weight loss, clinical steatorrhea, abnormal FE, vitamin deficiency, PFT, or other) were not used in any participants (n=0). Proportions are out of all participants with reported signs/symptoms (N=188).
Abbreviations: EPI, exocrine pancreatic insufficiency; FE, fecal elastase-1 test; PFT, pancreatic function testing.
All other combinations of the clinical symptoms/testing (weight loss, clinical steatorrhea, abnormal FE, vitamin deficiency, PFT, or other) were not used in any participants (n=0). Proportions are out of all participants with reported signs/symptoms (N=188).
Abbreviations: EPI, exocrine pancreatic insufficiency; FE, fecal elastase-1 test; PFT, pancreatic function testing.
Disclosures:
Rahul Pannala: HCL Technologies – Consultant. Nestle Healthsciences – Advisor or Review Panel Member.
Paramjit Benipal: fomat medical research – our medical group does research for above named company.
Kenneth Buch indicated no relevant financial relationships.
David Whitcomb: AbbVie – Consultant. Ariel Precison Medicine – Stock Options. CorEvitas, part of Thermo Fisher Scientific – Advisor or Review Panel Member. Nestlé Health Science – Advisor or Review Panel Member.
Jennifer Pack: Nestlé Health Science – Employee.
Janine Twal: Nestle Health Science – Employee, Stock-publicly held company(excluding mutual/index funds).
Jodie Barkin: Abbvie – Consultant. Aimmune Therapeutics – Consultant. Corevitas – Consultant. Exact Sciences – Consultant. Medtronic – Consultant. Motus GI – Consultant. Organon – Consultant.
Rahul Pannala, MD1, Paramjit Benipal, MD2, Kenneth L. Buch, MD3, David C.. Whitcomb, MD, PhD4, Jennifer Pack, MSN5, Janine Twal, PharmD5, Jodie A. Barkin, MD, FACG6, 54, Identifying Diagnostic Patterns for Exocrine Pancreatic Insufficiency in Adults With Chronic or Recurrent Acute Pancreatitis: Findings From the PACT-CP Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


