Endoscopy Video Forum
Annual Scientific Meeting
Session: Symposium 2C: Endoscopy Video Forum
V4 - Building Bridges: NOTES Salvage for EUS-Guided Gastroenterostomy
Monday, October 28, 2024
5:20 PM - 5:30 PM ET
Location: Terrace Ballroom 4

Carter E. Edmunds, MD (he/him/his)
University of Alabama at Birmingham Hospital
Birmingham, AL
Presenting Author - Endoscopy Video Forum(s)
Carter E. Edmunds, MD1, Dalton A.. Norwood, MD2, Babusai Rapaka, MD3, Jessica McCreight, 3, Rachel Mitchell, 3, Shajan Peter, MD3, Ali Ahmed, MD3, Kondal Kyanam, MD3, Ramzi Mulki, MD3, Sergio A. Sánchez-Luna, MD3
1University of Alabama at Birmingham Hospital, Birmingham, AL; 2UAB Minority Health & Health Equity Research Center, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) is an innovative procedure for palliating malignant gastric outlet obstruction. This procedure has been shown to have similar clinical outcomes to surgical GE with fewer adverse events (AEs). Despite this, complications are still possible with this procedure.
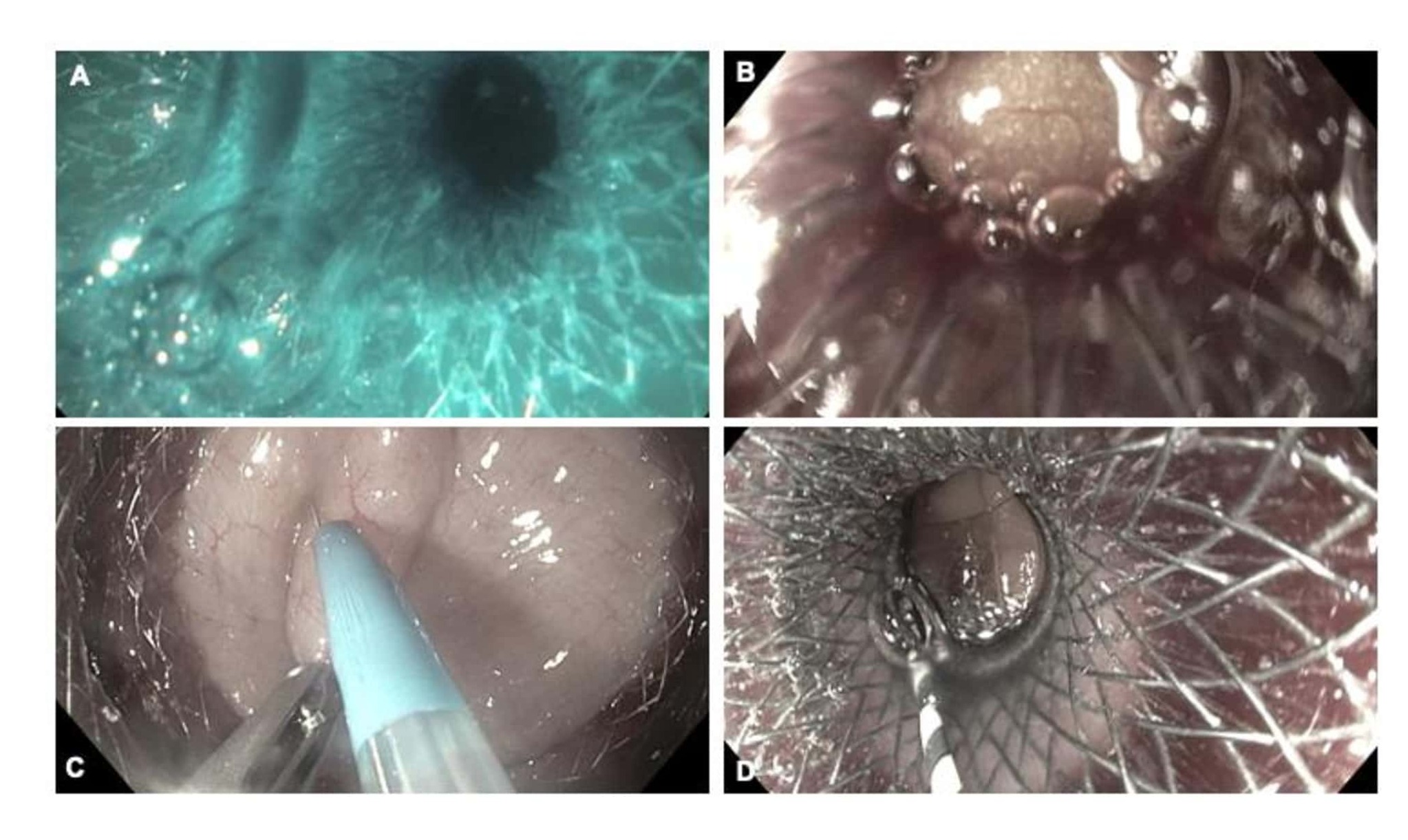
Case Description/Methods: A 75-year-old man presented with the inability to tolerate oral intake. Computed tomography scan demonstrated findings of concern for gastric outlet obstruction (GOO) secondary to a pancreas head mass with suspicious metastatic liver lesions. EUS-fine needle biopsy confirmed an unresectable pancreas adenocarcinoma; thus, we performed EUS-GE in the same session. A blue gush of Indigo Carmine and sterile saline was seen upon free-hand deployment of the proximal flange of the 20 mm x 10 mm lumen-apposing metal stent (LAMS) (Fig. 1A), suggesting jejunal access. Still, right after it, peritoneal fat was seen, indicating type I/type II stent misdeployment (Fig. 1B). A natural orifice transluminal endoscopic surgery (NOTES) technique for salvage was then performed. The peritoneal cavity was accessed after LAMS dilation with a through-the-scope (TTS) balloon dilator to 13.5 mm, and no enterotomy was appreciated on peritoneoscopy. Thus, using a double-channel endoscope, a loop of jejunum was grabbed and secured with a forceps. At the same time, a needle knife sphincterotome pre-loaded with a 0.035-inch 450 cm guide wire was used to perform an enterotomy (Fig. 1C), which was confirmed with an enterogram. Another 20 mm x 10 mm LAMS was used as a bridge between the jejunum and the other misdeployed LAMS (Fig. 1D). A 10 Fr x 4 cm double-pigtail plastic stent (DPPS) was placed to help with further anchoring of the 2 LAMSs. A computed tomography scan with oral contrast revealed no leak, and the patient recovered well. Repeat endoscopy at 4 weeks showed the EUS-GE with both LAMS still in an excellent position. The DPPS within the LAMS-in-LAMS bridge was removed. At 6 months of follow-up, the patient continues to do well with no GOO symptoms.
Discussion: As EUS-GE becomes increasingly popular as a palliative technique for GOO, it is essential to recognize potential complications of the procedure, such as the 4 types of LAMS misdeployment. The NOTES technique continues to be crucial as an endoscopic rescue method. It is imperative to use it when there is doubt about a type I vs. type II misdeployment, as an enterotomy needs closure to minimize further AEs, such as a leak and peritonitis.
Disclosures:
Carter E. Edmunds, MD1, Dalton A.. Norwood, MD2, Babusai Rapaka, MD3, Jessica McCreight, 3, Rachel Mitchell, 3, Shajan Peter, MD3, Ali Ahmed, MD3, Kondal Kyanam, MD3, Ramzi Mulki, MD3, Sergio A. Sánchez-Luna, MD3, V4, Building Bridges: NOTES Salvage for EUS-Guided Gastroenterostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham Hospital, Birmingham, AL; 2UAB Minority Health & Health Equity Research Center, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) is an innovative procedure for palliating malignant gastric outlet obstruction. This procedure has been shown to have similar clinical outcomes to surgical GE with fewer adverse events (AEs). Despite this, complications are still possible with this procedure.
Case Description/Methods: A 75-year-old man presented with the inability to tolerate oral intake. Computed tomography scan demonstrated findings of concern for gastric outlet obstruction (GOO) secondary to a pancreas head mass with suspicious metastatic liver lesions. EUS-fine needle biopsy confirmed an unresectable pancreas adenocarcinoma; thus, we performed EUS-GE in the same session. A blue gush of Indigo Carmine and sterile saline was seen upon free-hand deployment of the proximal flange of the 20 mm x 10 mm lumen-apposing metal stent (LAMS) (Fig. 1A), suggesting jejunal access. Still, right after it, peritoneal fat was seen, indicating type I/type II stent misdeployment (Fig. 1B). A natural orifice transluminal endoscopic surgery (NOTES) technique for salvage was then performed. The peritoneal cavity was accessed after LAMS dilation with a through-the-scope (TTS) balloon dilator to 13.5 mm, and no enterotomy was appreciated on peritoneoscopy. Thus, using a double-channel endoscope, a loop of jejunum was grabbed and secured with a forceps. At the same time, a needle knife sphincterotome pre-loaded with a 0.035-inch 450 cm guide wire was used to perform an enterotomy (Fig. 1C), which was confirmed with an enterogram. Another 20 mm x 10 mm LAMS was used as a bridge between the jejunum and the other misdeployed LAMS (Fig. 1D). A 10 Fr x 4 cm double-pigtail plastic stent (DPPS) was placed to help with further anchoring of the 2 LAMSs. A computed tomography scan with oral contrast revealed no leak, and the patient recovered well. Repeat endoscopy at 4 weeks showed the EUS-GE with both LAMS still in an excellent position. The DPPS within the LAMS-in-LAMS bridge was removed. At 6 months of follow-up, the patient continues to do well with no GOO symptoms.
Discussion: As EUS-GE becomes increasingly popular as a palliative technique for GOO, it is essential to recognize potential complications of the procedure, such as the 4 types of LAMS misdeployment. The NOTES technique continues to be crucial as an endoscopic rescue method. It is imperative to use it when there is doubt about a type I vs. type II misdeployment, as an enterotomy needs closure to minimize further AEs, such as a leak and peritonitis.
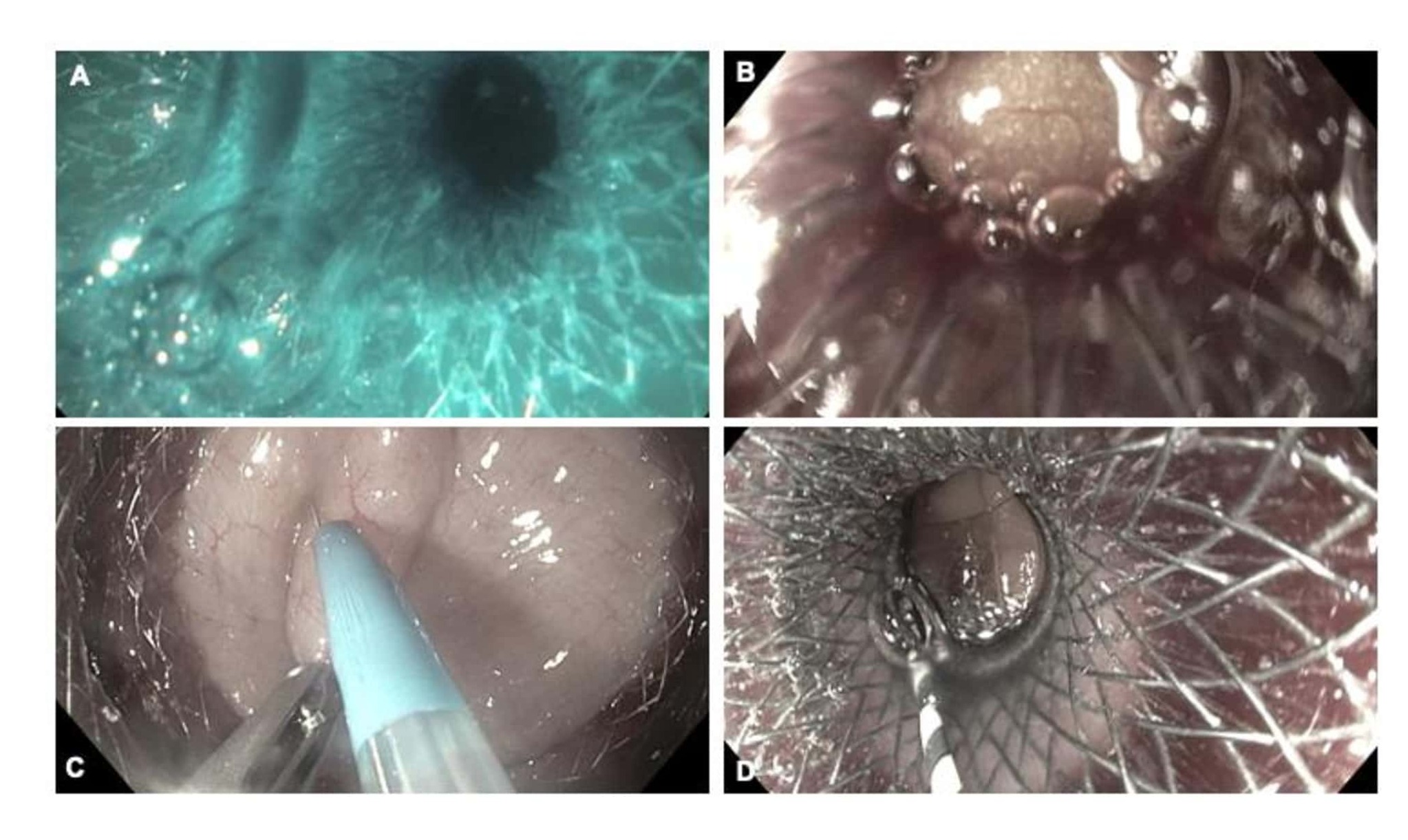
Figure: Figure 1. A) Blue gush of Indigo Carmine and sterile saline suggesting jejunal access of the distal flange of the lumen-apposing metal stent (LAMS) during endoscopic ultrasound (EUS)-guided gastroenterostomy; B) Misdeployed LAMS with proximal flange in the stomach and distal flange deployed in the peritoneum with peritoneal fat present distally suggesting type I vs. type II misdeployment; C) Natural orifice transluminal endoscopic surgery (NOTES) technique showing target jejunum loop fixated to the stomach wall with forceps while performing an enterotomy with a needle knife sphincterotome; D) LAMS-in-LAMS bridge showing an adequate connection between the jejunum and the stomach.
Disclosures:
Carter Edmunds indicated no relevant financial relationships.
Dalton Norwood indicated no relevant financial relationships.
Babusai Rapaka indicated no relevant financial relationships.
Jessica McCreight indicated no relevant financial relationships.
Rachel Mitchell indicated no relevant financial relationships.
Shajan Peter: Olympus – Consultant.
Ali Ahmed indicated no relevant financial relationships.
Kondal Kyanam indicated no relevant financial relationships.
Ramzi Mulki indicated no relevant financial relationships.
Sergio A. Sánchez-Luna indicated no relevant financial relationships.
Carter E. Edmunds, MD1, Dalton A.. Norwood, MD2, Babusai Rapaka, MD3, Jessica McCreight, 3, Rachel Mitchell, 3, Shajan Peter, MD3, Ali Ahmed, MD3, Kondal Kyanam, MD3, Ramzi Mulki, MD3, Sergio A. Sánchez-Luna, MD3, V4, Building Bridges: NOTES Salvage for EUS-Guided Gastroenterostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
