Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2B - Colon / General Endoscopy / GI Bleed / Practice Management
34 - Gastrointestinal Bleeding in Post-PCI Patients on Antiplatelet Therapy and the Predictive Value of the PRECISE-DAPT Score
Tuesday, October 29, 2024
9:30 AM - 9:40 AM ET
Location: Terrace Ballroom 2-3

Jesus Guzman, MD
Division of Gastroenterology, Department of Internal Medicine, Texas Tech University Health Sciences Center, El Paso, TX.
El Paso, Texas
Presenting Author(s)
Award: ACG Outstanding Research Award in the GI Bleeding Category (Trainee)
Jesus A. Guzman, MD1, Kahtan fadah, MD1, Kavita Gupta, MD1, Vishwajeet Singh, PhD1, Alok Dwivedi, PhD2, Debabrata Mukherjee, MD1, Kazue Okajima, MD1, Sherif E.. Elhanafi, MD1, Marc Zuckerman, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Dual antiplatelet therapy (DAPT) following percutaneous coronary intervention (PCI) in patients with acute coronary syndrome (ACS) mitigates the risk of thrombotic events. However, there is a significant risk of bleeding with DAPT, particularly gastrointestinal (GI) bleeding. Predicting Bleeding in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score has been used to predict bleeding during DAPT. We assessed the incidence of post-PCI GI bleeding in patients on DAPT, examining the diagnostic validity of the PRECISE-DAPT score for GI bleeding.
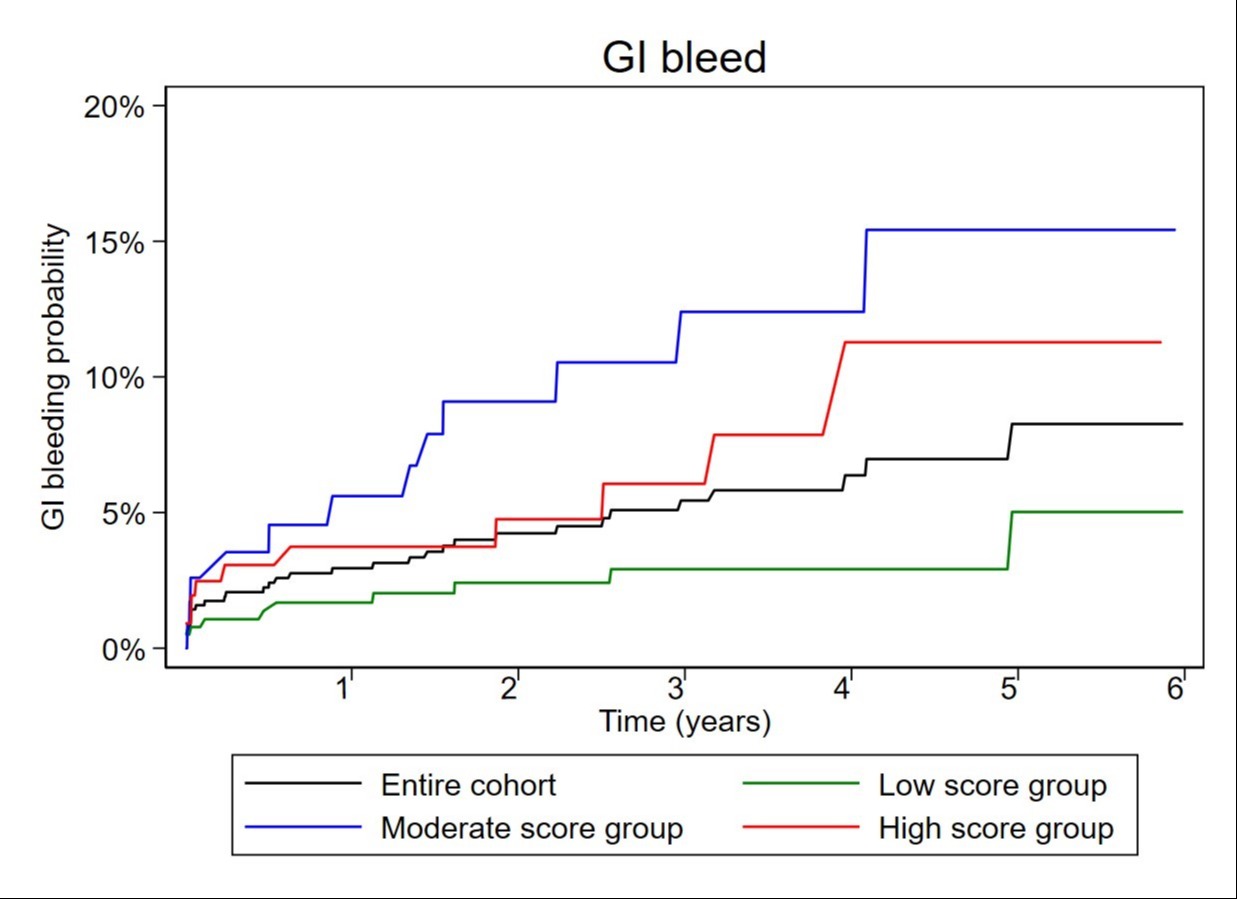
Methods: A retrospective cohort study was conducted on patients receiving DAPT post-PCI from 2014 to 2021. The primary objective was to determine the GI bleeding rate at one year and for the entire study period. Endoscopic indications, findings, concurrent antiplatelet therapy, and primary cause of bleeding were recorded. Secondary objective was to evaluate the predictive value of the PRECISE-DAPT score, categorized into low (≤17), moderate (18 to 24), and high (≥25). We applied the Kaplan-Meier method, log-rank test, and Cox hazards regression to estimate time to GI incidence and hazard ratio (HR) with a 95% confidence interval (CI).
Results: We included a cohort of 1067 patients, with a mean age of 62.3 years, predominantly male (66.6%), and Hispanic (77.1%). Of these, 563 patients (57.9%) received clopidogrel, and 409 (42%) received ticagrelor. The GI bleeding rate at one year was 2.5%, and 3.6% (39 patients) for the total study period with a median follow-up of 2.2 years (IQR 0.2, 4.2). Among the GI bleeds, lower GI bleeding accounted for 44 %, upper GI bleeding 31%, small bowel bleeding 10%, undetermined 15% with the most frequent etiology being colon cancer (18%). Propensity score-matched analysis indicated no significant difference in GI bleeding between the clopidogrel and ticagrelor groups (21.2% vs. 19.2%, HR: 0.6, 95% CI: 0.3-1.3, p=0.2). In the propensity score-matched data, the odds of GI bleeding were significantly higher in patients with high-risk (OR: 2.5; 95% CI: 1, 6) and moderate-risk (OR: 2.8; 95% CI: 1.1, 7.2) PRECISE-DAPT scores compared to those with low-risk scores.
Discussion: In a predominantly Hispanic population, the bleeding rate post-PCI on DAPT was 2.5 %. Incidental colon cancers were identified as the most frequent cause of bleeding. This study found the PRECISE-DAPT score was useful in predicting GI bleeding risk in patients on DAPT post-PCI.
Disclosures:
Jesus A. Guzman, MD1, Kahtan fadah, MD1, Kavita Gupta, MD1, Vishwajeet Singh, PhD1, Alok Dwivedi, PhD2, Debabrata Mukherjee, MD1, Kazue Okajima, MD1, Sherif E.. Elhanafi, MD1, Marc Zuckerman, MD1, 34, Gastrointestinal Bleeding in Post-PCI Patients on Antiplatelet Therapy and the Predictive Value of the PRECISE-DAPT Score, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Jesus A. Guzman, MD1, Kahtan fadah, MD1, Kavita Gupta, MD1, Vishwajeet Singh, PhD1, Alok Dwivedi, PhD2, Debabrata Mukherjee, MD1, Kazue Okajima, MD1, Sherif E.. Elhanafi, MD1, Marc Zuckerman, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Dual antiplatelet therapy (DAPT) following percutaneous coronary intervention (PCI) in patients with acute coronary syndrome (ACS) mitigates the risk of thrombotic events. However, there is a significant risk of bleeding with DAPT, particularly gastrointestinal (GI) bleeding. Predicting Bleeding in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score has been used to predict bleeding during DAPT. We assessed the incidence of post-PCI GI bleeding in patients on DAPT, examining the diagnostic validity of the PRECISE-DAPT score for GI bleeding.
Methods: A retrospective cohort study was conducted on patients receiving DAPT post-PCI from 2014 to 2021. The primary objective was to determine the GI bleeding rate at one year and for the entire study period. Endoscopic indications, findings, concurrent antiplatelet therapy, and primary cause of bleeding were recorded. Secondary objective was to evaluate the predictive value of the PRECISE-DAPT score, categorized into low (≤17), moderate (18 to 24), and high (≥25). We applied the Kaplan-Meier method, log-rank test, and Cox hazards regression to estimate time to GI incidence and hazard ratio (HR) with a 95% confidence interval (CI).
Results: We included a cohort of 1067 patients, with a mean age of 62.3 years, predominantly male (66.6%), and Hispanic (77.1%). Of these, 563 patients (57.9%) received clopidogrel, and 409 (42%) received ticagrelor. The GI bleeding rate at one year was 2.5%, and 3.6% (39 patients) for the total study period with a median follow-up of 2.2 years (IQR 0.2, 4.2). Among the GI bleeds, lower GI bleeding accounted for 44 %, upper GI bleeding 31%, small bowel bleeding 10%, undetermined 15% with the most frequent etiology being colon cancer (18%). Propensity score-matched analysis indicated no significant difference in GI bleeding between the clopidogrel and ticagrelor groups (21.2% vs. 19.2%, HR: 0.6, 95% CI: 0.3-1.3, p=0.2). In the propensity score-matched data, the odds of GI bleeding were significantly higher in patients with high-risk (OR: 2.5; 95% CI: 1, 6) and moderate-risk (OR: 2.8; 95% CI: 1.1, 7.2) PRECISE-DAPT scores compared to those with low-risk scores.
Discussion: In a predominantly Hispanic population, the bleeding rate post-PCI on DAPT was 2.5 %. Incidental colon cancers were identified as the most frequent cause of bleeding. This study found the PRECISE-DAPT score was useful in predicting GI bleeding risk in patients on DAPT post-PCI.
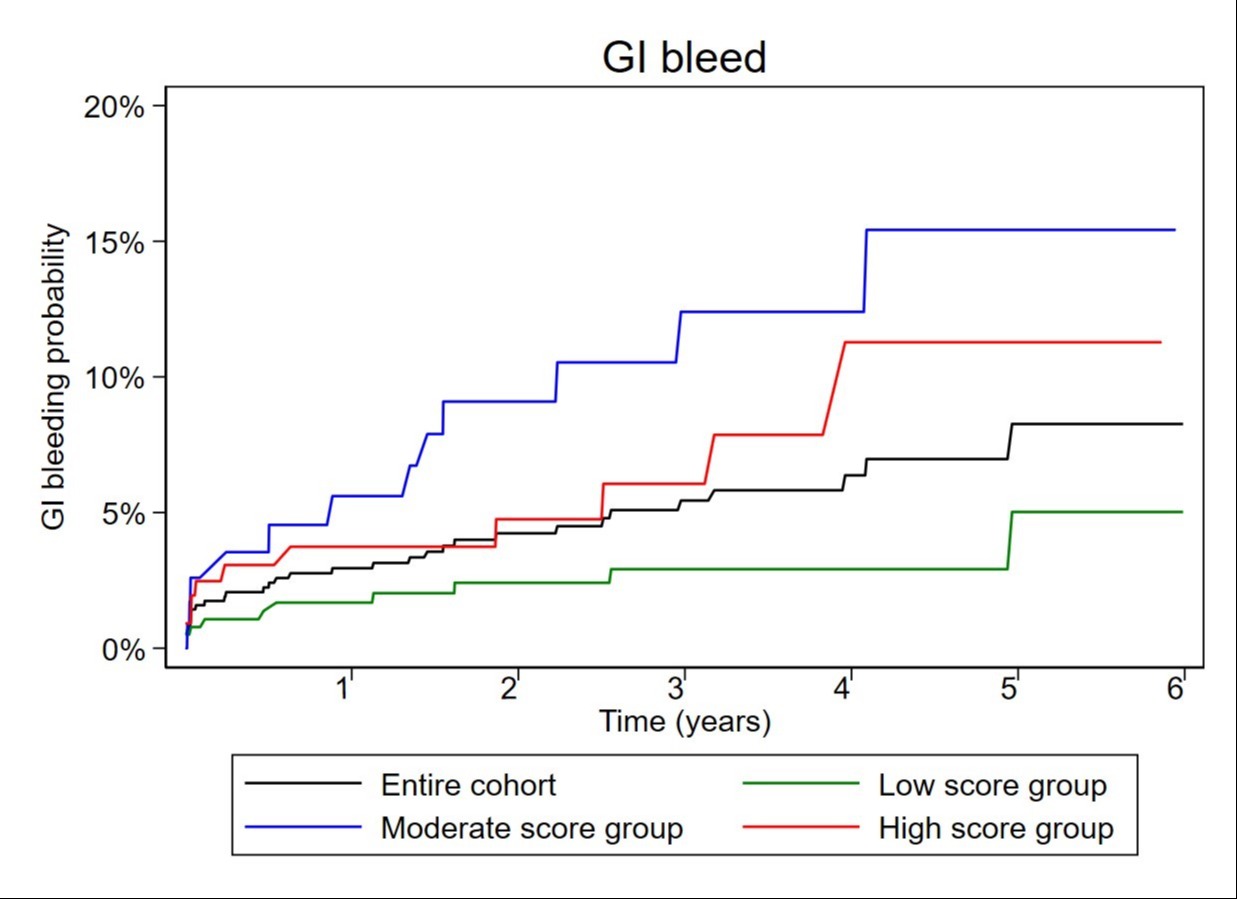
Figure: Time to GI bleeding Kaplan Meier curve
Disclosures:
Jesus Guzman indicated no relevant financial relationships.
Kahtan fadah indicated no relevant financial relationships.
Kavita Gupta indicated no relevant financial relationships.
Vishwajeet Singh indicated no relevant financial relationships.
Alok Dwivedi indicated no relevant financial relationships.
Debabrata Mukherjee indicated no relevant financial relationships.
Kazue Okajima indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Marc Zuckerman indicated no relevant financial relationships.
Jesus A. Guzman, MD1, Kahtan fadah, MD1, Kavita Gupta, MD1, Vishwajeet Singh, PhD1, Alok Dwivedi, PhD2, Debabrata Mukherjee, MD1, Kazue Okajima, MD1, Sherif E.. Elhanafi, MD1, Marc Zuckerman, MD1, 34, Gastrointestinal Bleeding in Post-PCI Patients on Antiplatelet Therapy and the Predictive Value of the PRECISE-DAPT Score, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.



