Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2B - Colon / General Endoscopy / GI Bleed / Practice Management
35 - Compliance Rate of Discharging Post Variceal Bleed Patients on Non-Selective Beta Blocker: A Quality Improvement Project
Tuesday, October 29, 2024
9:40 AM - 9:50 AM ET
Location: Terrace Ballroom 2-3

Haider Ghazanfar, MD (he/him/his)
BronxCare Health System
Bronx, NY
Presenting Author(s)
Award: ACG Auxiliary Award (Trainee)
Haider Ghazanfar, MD1, Sameer Kandhi, MD1, Franklin Sosa, MD1, Ali Ghazanfar, MBBS2, Harish Patel, MD1
1BronxCare Health System, Bronx, NY; 2Fauji Foundation Hospital, Rawalpindi, Punjab, Pakistan
Introduction: Esophageal varices bleeding carries a significantly high mortality in patients with liver cirrhosis. Non-selective beta-blockers have been shown to prevent re-bleeding in patients with esophageal varices banding. Post banding patients are often octreotide and then transitioned to b-blockers. Compliance often lapsed during this transition. Quality improvement projects are frequently performed to check compliance and identify optimal implementation methods. Here we present improvement in the quality measure after a gastroenterology fellow led a quality improvement project.
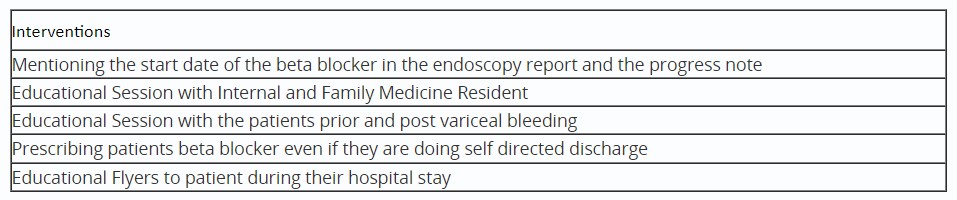
Methods: The Quality Improvement Project was done in two phases. The first phase involved doing a retrospective chart review of patients who underwent variceal banding as inpatients over 3 months to assess the compliance rate of discharging these patients on non-selective beta blockers and to formulate strategies to improve the compliance rate. Based on the information collected during the first phase four interventions were implemented in the following two years from July 2022 to June 2024. Implementation made in the study included mentioning the start date of the beta-blocker in the endoscopy report and the gastroenterology progress note, evening reports with internal and family medicine residents regarding the importance of initiating beta blockers in patients with variceal bleeding, educating patients regarding the importance of beta-blocker and follow up after variceal bleeding episodes, prescribing patients beta-blocker to patient even if they are doing self-directed discharges and giving educational flyers for the patients during their hospital stay. The house-staff survey was done to determine the best method that impacted compliance.
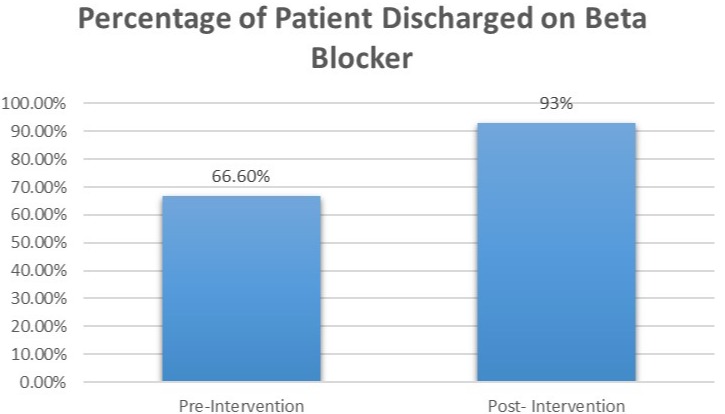
Results: The compliance of discharging post-variceal bleeding patients with no contraindication before the intervention was 66%. The compliance rate of discharging post-variceal bleeding patients with no contraindication went up to 93% after the interventions from the quality improvement project. It has been presented in Figure 1. The house staff survey summarized that documentation of the precise date of the starting b-blocker had a large impact on assuring compliance.
Discussion: Quality improvement projects do assist in improving the outcomes. The precise documentation of the start date of the non-selective b-blocker in patients with esophageal varices banding was found to be the best measure in increasing compliance rate of discharging patients on beta-blockers.
Disclosures:
Haider Ghazanfar, MD1, Sameer Kandhi, MD1, Franklin Sosa, MD1, Ali Ghazanfar, MBBS2, Harish Patel, MD1, 35, Compliance Rate of Discharging Post Variceal Bleed Patients on Non-Selective Beta Blocker: A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Haider Ghazanfar, MD1, Sameer Kandhi, MD1, Franklin Sosa, MD1, Ali Ghazanfar, MBBS2, Harish Patel, MD1
1BronxCare Health System, Bronx, NY; 2Fauji Foundation Hospital, Rawalpindi, Punjab, Pakistan
Introduction: Esophageal varices bleeding carries a significantly high mortality in patients with liver cirrhosis. Non-selective beta-blockers have been shown to prevent re-bleeding in patients with esophageal varices banding. Post banding patients are often octreotide and then transitioned to b-blockers. Compliance often lapsed during this transition. Quality improvement projects are frequently performed to check compliance and identify optimal implementation methods. Here we present improvement in the quality measure after a gastroenterology fellow led a quality improvement project.
Methods: The Quality Improvement Project was done in two phases. The first phase involved doing a retrospective chart review of patients who underwent variceal banding as inpatients over 3 months to assess the compliance rate of discharging these patients on non-selective beta blockers and to formulate strategies to improve the compliance rate. Based on the information collected during the first phase four interventions were implemented in the following two years from July 2022 to June 2024. Implementation made in the study included mentioning the start date of the beta-blocker in the endoscopy report and the gastroenterology progress note, evening reports with internal and family medicine residents regarding the importance of initiating beta blockers in patients with variceal bleeding, educating patients regarding the importance of beta-blocker and follow up after variceal bleeding episodes, prescribing patients beta-blocker to patient even if they are doing self-directed discharges and giving educational flyers for the patients during their hospital stay. The house-staff survey was done to determine the best method that impacted compliance.
Results: The compliance of discharging post-variceal bleeding patients with no contraindication before the intervention was 66%. The compliance rate of discharging post-variceal bleeding patients with no contraindication went up to 93% after the interventions from the quality improvement project. It has been presented in Figure 1. The house staff survey summarized that documentation of the precise date of the starting b-blocker had a large impact on assuring compliance.
Discussion: Quality improvement projects do assist in improving the outcomes. The precise documentation of the start date of the non-selective b-blocker in patients with esophageal varices banding was found to be the best measure in increasing compliance rate of discharging patients on beta-blockers.
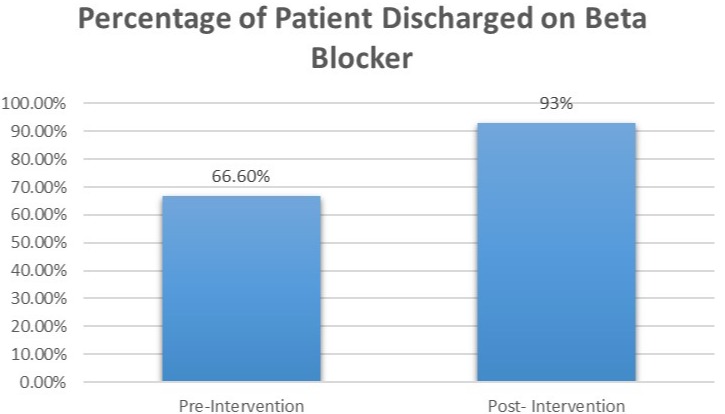
Figure: Percentage of Patient Discharged Beta Blocker Pre and Post Intervention
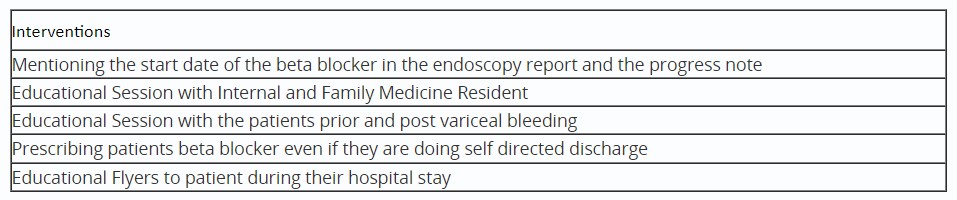
Table: Intervention Implemented to increase the compliance rate of discharging post variceal bleed patients on non-selective beta blocker
Disclosures:
Haider Ghazanfar indicated no relevant financial relationships.
Sameer Kandhi indicated no relevant financial relationships.
Franklin Sosa indicated no relevant financial relationships.
Ali Ghazanfar indicated no relevant financial relationships.
Harish Patel indicated no relevant financial relationships.
Haider Ghazanfar, MD1, Sameer Kandhi, MD1, Franklin Sosa, MD1, Ali Ghazanfar, MBBS2, Harish Patel, MD1, 35, Compliance Rate of Discharging Post Variceal Bleed Patients on Non-Selective Beta Blocker: A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.



