Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3A - Esophagus / Stomach / Practice Management
38 - Abnormal Secondary Peristalsis Demonstrated by FLIP Panometry is Frequently Seen in Patients With Normal Peristalsis on High-Resolution Manometry
Tuesday, October 29, 2024
2:25 PM - 2:35 PM ET
Location: Terrace Ballroom 1

Rhea Fogla, MD (she/her/hers)
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Rhea Fogla, MD1, Gaurav Ghosh, MD2, Michelle Lee, MD3, Felice Schnoll-Sussman, MD1, Philip Katz, MD4
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian Hospita/Weill Cornell, New York, NY; 3New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 4Weill Cornell Medicine, New York, NY
Introduction: Functional luminal imaging probe (FLIP) panometry assesses secondary peristalsis. High resolution manometry (HRM) assesses primary peristalsis. Current data supports that normal FLIP panometry is associated with normal peristalsis on HRM, but whether abnormal FLIP panometry reflects abnormal peristalsis on HRM is less clear. The aim of this study is to investigate the relationship of abnormal FLIP panometry with esophageal body contraction patterns on HRM, as defined by Chicago Classification 4.0 (CCv4).
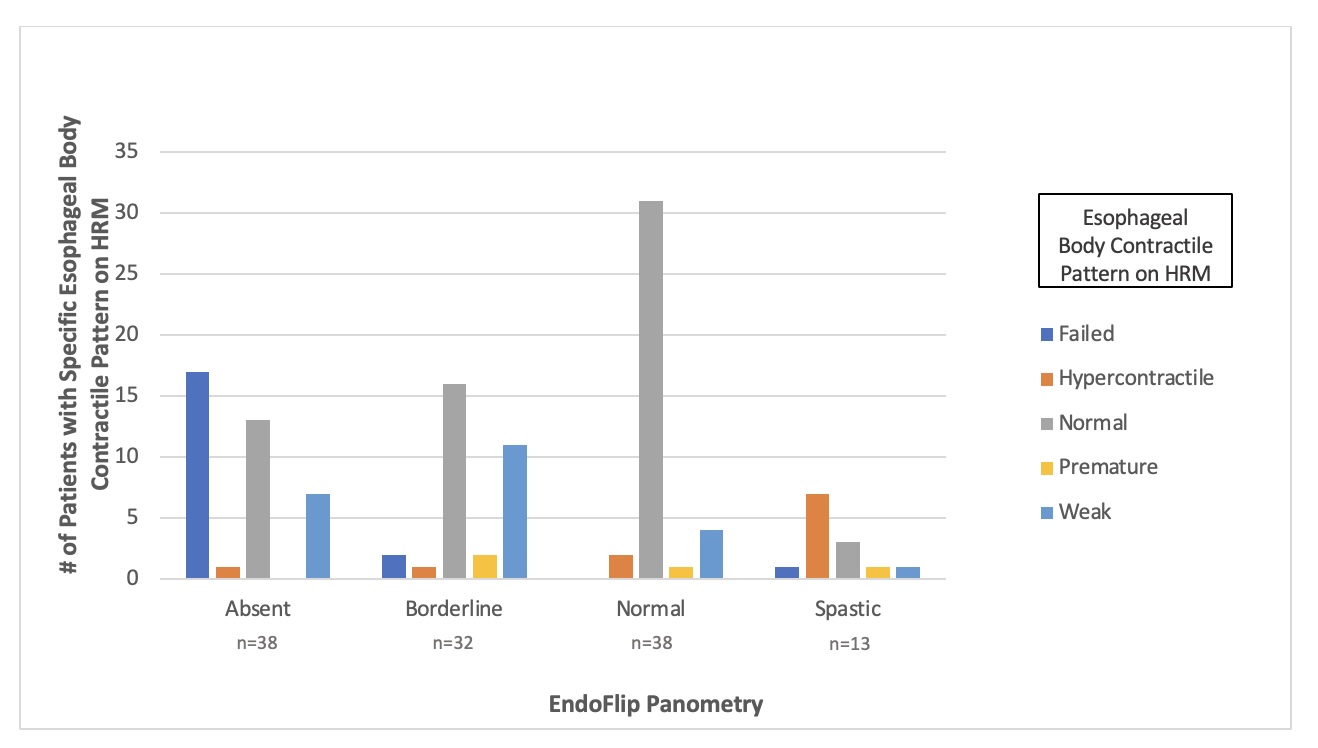
Methods: This is a retrospective observational study of patients presenting to NYP-Weill Cornell from 6/2020 to 6/2022 who had 16cm FLIP and HRM within one year. Patients were included if they had analyzable data for maximum esophagogastric junction (EGJ) diameter, distensibility index at 60 mL fill, and panometry. Panometry was classified as normal, borderline, absent, or spastic as previously described (Fig 1). HRM was classified based on CCv4. Studies were reviewed and findings agreed upon by two experienced gastroenterologists.
Results: 121 adults (61% female, mean age 56.8 years) were included; 40 patients were evaluated with FLIP and HRM the same day. 38 patients (31%) had normal panometry and of those, 82% had normal peristalsis on HRM (Fig 1). 38 patients had absent contractility on panometry: 21 of these patients (55%) had evidence of some normal peristalsis on HRM (13 normal, 7 weak, 1 hypercontractile). 31/121 (26%) had panometric findings discordant with esophageal body contraction pattern on HRM. FLIP panometry and HRM contractility was frequently discordant in the setting of an elevated IRP on HRM (p< 0.001, Chi-squared test). Discordance was not seen with reduced or borderline EGJ opening on FLIP (p=0.184).
Discussion: Summary:
This study confirms that normal secondary peristalsis seen on FLIP panometry is associated with normal primary peristalsis on HRM. However, normal primary peristalsis may be seen in the setting of abnormal secondary peristalsis on FLIP panometry.
Conclusion:
Our data suggests that abnormal secondary peristalsis may be found in patients with normal primary peristalsis. Given the discordant findings between FLIP panometry and HRM, abnormal panometry at this time should be followed by HRM, as both results may be clinically relevant.
Disclosures:
Rhea Fogla, MD1, Gaurav Ghosh, MD2, Michelle Lee, MD3, Felice Schnoll-Sussman, MD1, Philip Katz, MD4, 38, Abnormal Secondary Peristalsis Demonstrated by FLIP Panometry is Frequently Seen in Patients With Normal Peristalsis on High-Resolution Manometry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian Hospita/Weill Cornell, New York, NY; 3New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 4Weill Cornell Medicine, New York, NY
Introduction: Functional luminal imaging probe (FLIP) panometry assesses secondary peristalsis. High resolution manometry (HRM) assesses primary peristalsis. Current data supports that normal FLIP panometry is associated with normal peristalsis on HRM, but whether abnormal FLIP panometry reflects abnormal peristalsis on HRM is less clear. The aim of this study is to investigate the relationship of abnormal FLIP panometry with esophageal body contraction patterns on HRM, as defined by Chicago Classification 4.0 (CCv4).
Methods: This is a retrospective observational study of patients presenting to NYP-Weill Cornell from 6/2020 to 6/2022 who had 16cm FLIP and HRM within one year. Patients were included if they had analyzable data for maximum esophagogastric junction (EGJ) diameter, distensibility index at 60 mL fill, and panometry. Panometry was classified as normal, borderline, absent, or spastic as previously described (Fig 1). HRM was classified based on CCv4. Studies were reviewed and findings agreed upon by two experienced gastroenterologists.
Results: 121 adults (61% female, mean age 56.8 years) were included; 40 patients were evaluated with FLIP and HRM the same day. 38 patients (31%) had normal panometry and of those, 82% had normal peristalsis on HRM (Fig 1). 38 patients had absent contractility on panometry: 21 of these patients (55%) had evidence of some normal peristalsis on HRM (13 normal, 7 weak, 1 hypercontractile). 31/121 (26%) had panometric findings discordant with esophageal body contraction pattern on HRM. FLIP panometry and HRM contractility was frequently discordant in the setting of an elevated IRP on HRM (p< 0.001, Chi-squared test). Discordance was not seen with reduced or borderline EGJ opening on FLIP (p=0.184).
Discussion: Summary:
This study confirms that normal secondary peristalsis seen on FLIP panometry is associated with normal primary peristalsis on HRM. However, normal primary peristalsis may be seen in the setting of abnormal secondary peristalsis on FLIP panometry.
Conclusion:
Our data suggests that abnormal secondary peristalsis may be found in patients with normal primary peristalsis. Given the discordant findings between FLIP panometry and HRM, abnormal panometry at this time should be followed by HRM, as both results may be clinically relevant.
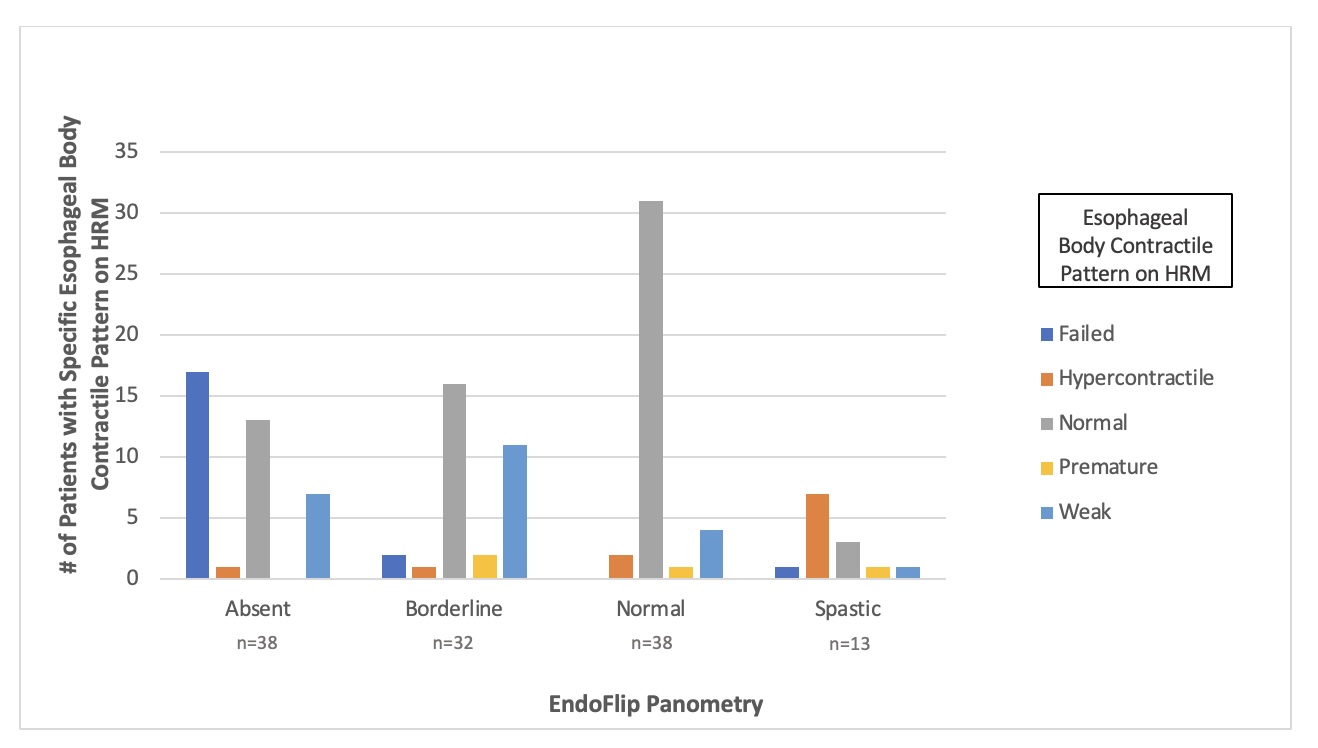
Figure: Figure 1. Relationship between Endoflip panometry and esophageal motility patterns on HRM. Eight-two percent of patients with normal panometry had normal contractile pattern on HRM. Fifty-five percent with absent contractility had evidence of peristalsis on HRM. FLIP Panometry is categorized as normal, borderline, absent, or spastic. Normal Contractile Response requires >/= 6 consecutive repetitive antegrade contraction (RACs). Borderline contractile response is defined as < 6 consecutive RACs, though may have distinct or sporadic contractions and does not meet requirements for spastic contractile response. Absent contractile response is defined as no contractile activity. Spastic contractile response is defined as sustained occluding contractions, sustained lower esophageal sphincter contractions, or repetitive retrograde contractions.
Disclosures:
Rhea Fogla indicated no relevant financial relationships.
Gaurav Ghosh: Phathom Pharmaceuticals – Consultant.
Michelle Lee indicated no relevant financial relationships.
Felice Schnoll-Sussman: Ethicon – Consultant. Phathom Pharmaceuticals – Consultant. Sebella – Consultant.
Philip Katz: Phathom Pharmaceuticals – Consultant. Sebella – Consultant.
Rhea Fogla, MD1, Gaurav Ghosh, MD2, Michelle Lee, MD3, Felice Schnoll-Sussman, MD1, Philip Katz, MD4, 38, Abnormal Secondary Peristalsis Demonstrated by FLIP Panometry is Frequently Seen in Patients With Normal Peristalsis on High-Resolution Manometry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

