Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3A - Esophagus / Stomach / Practice Management
39 - Incidence of Young-Onset Barrett’s Esophagus is Increasing: A Population-Based Study From a Multi-Institutional National Database
Tuesday, October 29, 2024
2:35 PM - 2:45 PM ET
Location: Terrace Ballroom 1

Anila Vasireddy, MD (she/her/hers)
University of Pennsylvania Health System
Philadelphia, PA
Presenting Author(s)
Anila Vasireddy, MD1, Apoorva K. Chandar, MBBS, MPH2, Mart Andrew Maravillas, MS3, Jaime A. Perez, PhD4, Sandra Algarin Perneth, MD5, Cadman Leggett, MD5, Prasad G. Iyer, MD, MS, FACG6, Srinivas Gaddam, MD, MPH7, Amrit K.. Kamboj, MD7
1University of Pennsylvania Health System, Philadelphia, PA; 2Case Western Reserve University School of Medicine, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Akron, OH; 4University Hospitals Clinical Research Center, Cleveland, OH; 5Mayo Clinic, Rochester, MN; 6Mayo Clinic, Phoenix, AZ; 7Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Esophageal adenocarcinoma (EAC), a cancer with rising incidence and presenting at advanced stages in younger patients (< 50 years) compared to > 50 years. We aimed to examine the epidemiology of young-onset Barrett’s esophagus (BE) (< age 50), including its incidence, trends, and risk factors, using a large national database.
Methods: Data was extracted from the TriNetX database, a composite of electronic health records from 88 healthcare organizations, from inception to November 2023. BE was defined using ICD-9/10 and encompassed non-dysplastic BE (NDBE), dysplastic BE, and EAC. BE patients were required to have a negative EGD prior to index BE diagnosis. Controls were patients without BE. For both cases and controls, data was extracted on conventional BE risk factors including age, sex, race, gastroesophageal reflux disease (GERD) symptoms, body mass index (BMI), smoking, hiatal hernia, and obstructive sleep apnea (OSA). Patients were further stratified by age (young, < 50 years; old, ≥50 years). Categorical and continuous variables were analyzed using the Pearson’s chi-squared test and Welch’s t-test respectively. Joinpoint regression was used to evaluate trends. Logistic regression was used to evaluate for independent predictors of young-onset BE.
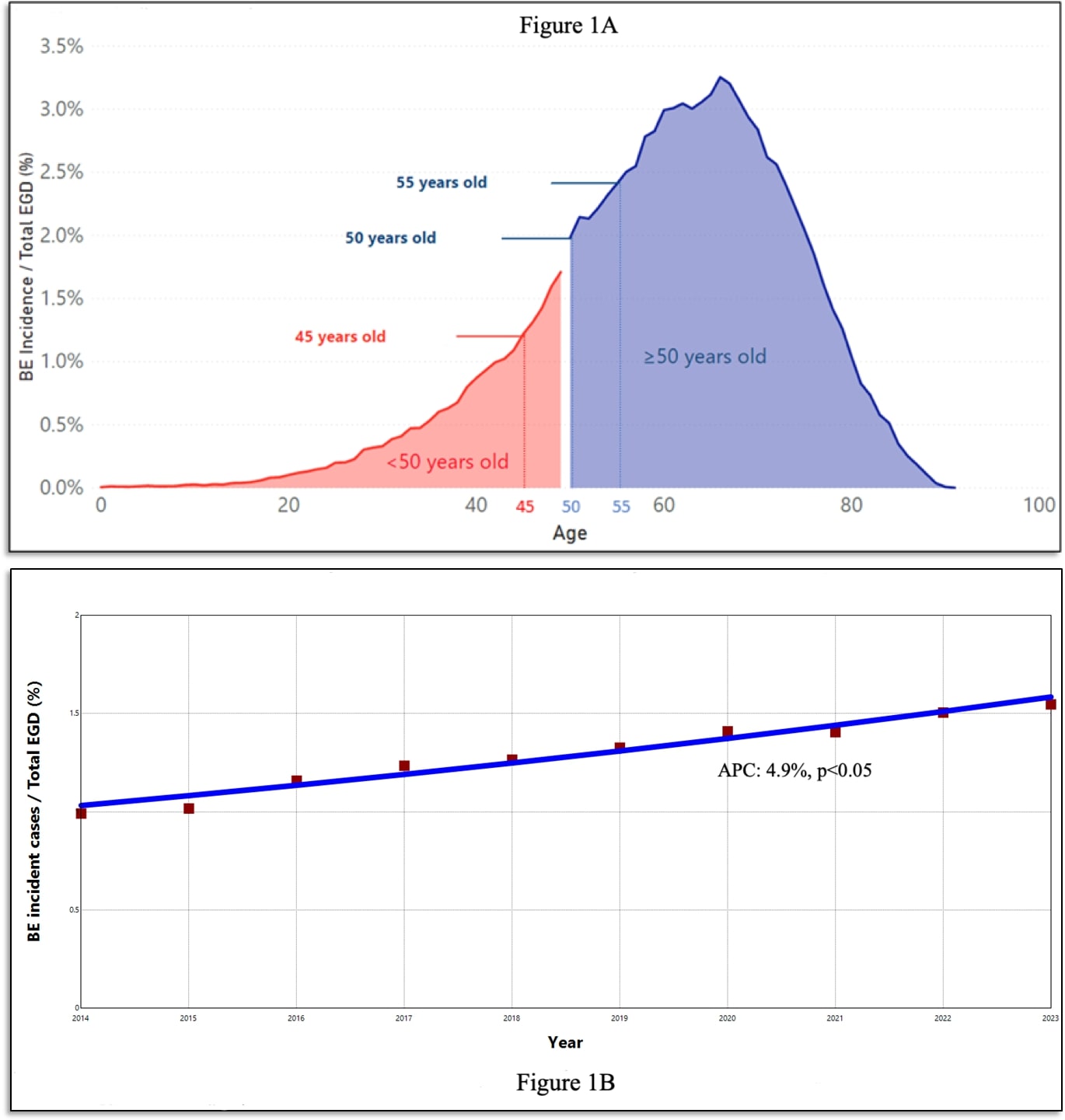
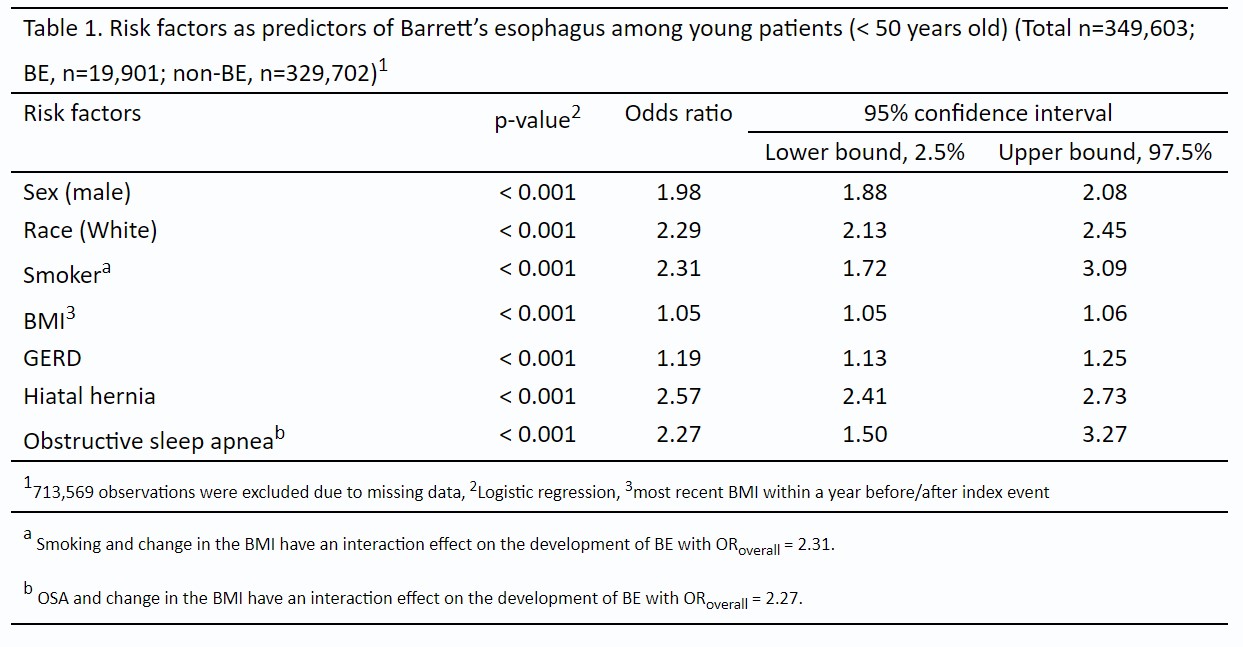
Results: A total of 2,670,143 patients were included (Incident BE - 102,598 (3.8%) [young, < 50 years, n=19,901 (1.9%); old, ≥50 years, n=79,686 (5.2%)]. Young-onset BE accounted for 20% of all incident BE cases. Majority had NDBE at initial diagnosis (n=18,612, 94%). Incidence of BE in 45-49 year and 50-54-year age groups were not clinically significant (2.3% vs. 2.6%, p< 0.05). A significantly increasing trend of young-onset BE was seen from 2014 to 2023 on Joinpoint regression (p< 0.05) (Figure 1B). Hiatal hernia (OR 2.6), smoking (OR 2.3), White race (OR 2.3), OSA (OR 2.2), male sex (OR 2.0), GERD symptoms (OR 1.2), and BMI (OR 1.1) were independent predictors of young-onset BE (Table 1).
Discussion: In a large population-based study, we show that 20% of patients had BE incidence before the age of 50, with an increasing trend over the last decade. An alarming 6% of young-onset BE had BE-related neoplasia. The incidence of BE in the 45 – 50 age-group is nearly the same as that of 50 – 55 age-group (2.3% vs 2.6%). Our study validates that conventional risk-factors of BE in older patients also predict young-onset BE. Screening for BE before the age of 50 may have a significant impact on early detection of EAC.
Disclosures:
Anila Vasireddy, MD1, Apoorva K. Chandar, MBBS, MPH2, Mart Andrew Maravillas, MS3, Jaime A. Perez, PhD4, Sandra Algarin Perneth, MD5, Cadman Leggett, MD5, Prasad G. Iyer, MD, MS, FACG6, Srinivas Gaddam, MD, MPH7, Amrit K.. Kamboj, MD7, 39, Incidence of Young-Onset Barrett’s Esophagus is Increasing: A Population-Based Study From a Multi-Institutional National Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Pennsylvania Health System, Philadelphia, PA; 2Case Western Reserve University School of Medicine, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Akron, OH; 4University Hospitals Clinical Research Center, Cleveland, OH; 5Mayo Clinic, Rochester, MN; 6Mayo Clinic, Phoenix, AZ; 7Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Esophageal adenocarcinoma (EAC), a cancer with rising incidence and presenting at advanced stages in younger patients (< 50 years) compared to > 50 years. We aimed to examine the epidemiology of young-onset Barrett’s esophagus (BE) (< age 50), including its incidence, trends, and risk factors, using a large national database.
Methods: Data was extracted from the TriNetX database, a composite of electronic health records from 88 healthcare organizations, from inception to November 2023. BE was defined using ICD-9/10 and encompassed non-dysplastic BE (NDBE), dysplastic BE, and EAC. BE patients were required to have a negative EGD prior to index BE diagnosis. Controls were patients without BE. For both cases and controls, data was extracted on conventional BE risk factors including age, sex, race, gastroesophageal reflux disease (GERD) symptoms, body mass index (BMI), smoking, hiatal hernia, and obstructive sleep apnea (OSA). Patients were further stratified by age (young, < 50 years; old, ≥50 years). Categorical and continuous variables were analyzed using the Pearson’s chi-squared test and Welch’s t-test respectively. Joinpoint regression was used to evaluate trends. Logistic regression was used to evaluate for independent predictors of young-onset BE.
Results: A total of 2,670,143 patients were included (Incident BE - 102,598 (3.8%) [young, < 50 years, n=19,901 (1.9%); old, ≥50 years, n=79,686 (5.2%)]. Young-onset BE accounted for 20% of all incident BE cases. Majority had NDBE at initial diagnosis (n=18,612, 94%). Incidence of BE in 45-49 year and 50-54-year age groups were not clinically significant (2.3% vs. 2.6%, p< 0.05). A significantly increasing trend of young-onset BE was seen from 2014 to 2023 on Joinpoint regression (p< 0.05) (Figure 1B). Hiatal hernia (OR 2.6), smoking (OR 2.3), White race (OR 2.3), OSA (OR 2.2), male sex (OR 2.0), GERD symptoms (OR 1.2), and BMI (OR 1.1) were independent predictors of young-onset BE (Table 1).
Discussion: In a large population-based study, we show that 20% of patients had BE incidence before the age of 50, with an increasing trend over the last decade. An alarming 6% of young-onset BE had BE-related neoplasia. The incidence of BE in the 45 – 50 age-group is nearly the same as that of 50 – 55 age-group (2.3% vs 2.6%). Our study validates that conventional risk-factors of BE in older patients also predict young-onset BE. Screening for BE before the age of 50 may have a significant impact on early detection of EAC.
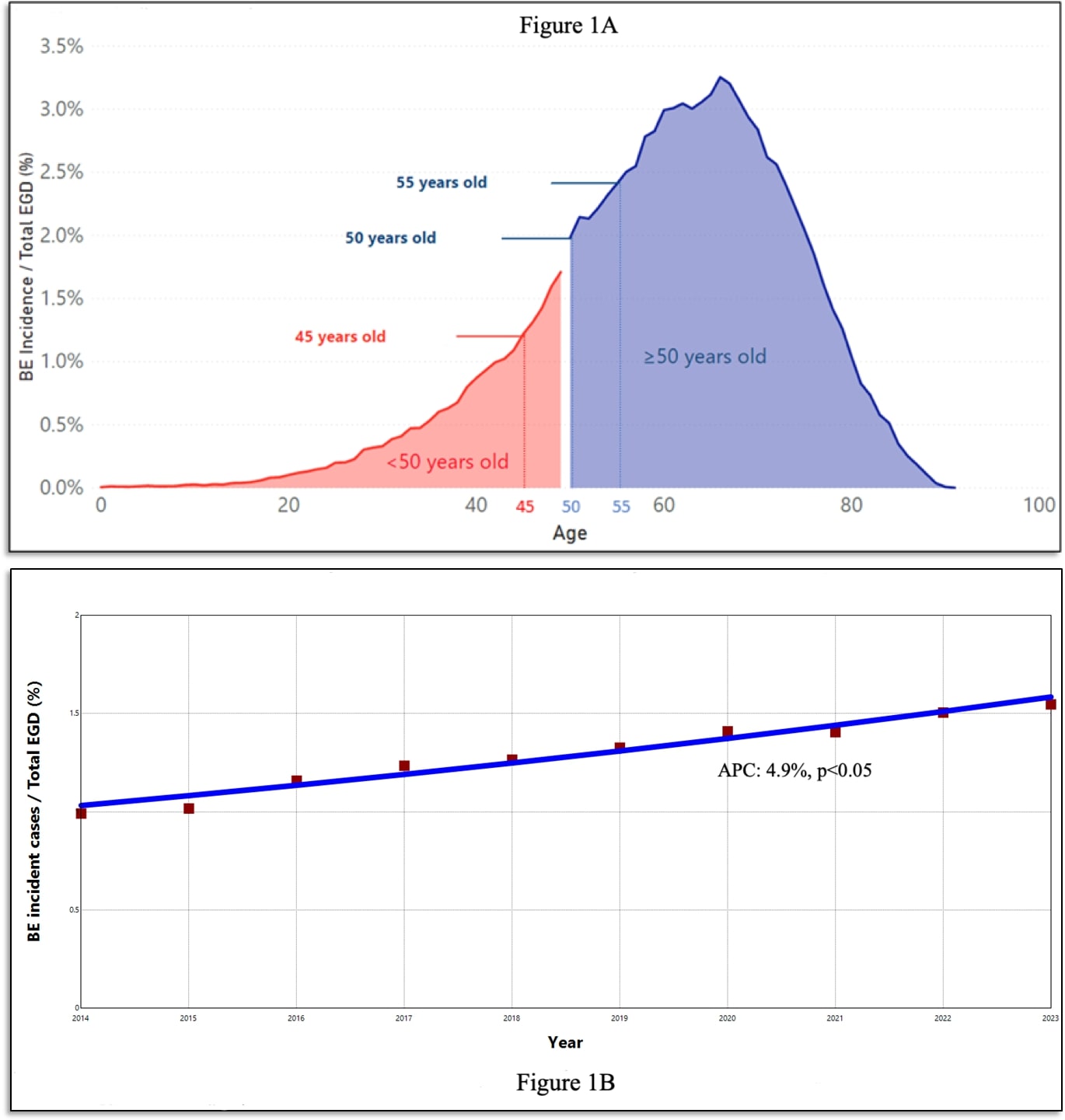
Figure: Figure 1. A) Distribution of BE incident cases by age. B) Trends in incidence of young-onset BE between 2014-2023.
Disclosures:
Anila Vasireddy indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Mart Andrew Maravillas indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Sandra Algarin Perneth indicated no relevant financial relationships.
Cadman Leggett: Castle Biosciences – Consultant.
Prasad G. Iyer: Castle Biosciences – Consultant, Grant/Research Support. CDx Medical – Consultant, Grant/Research Support. Exact Sciences – Advisory Committee/Board Member, Consultant, Grant/Research Support, Intellectual Property/Patents. Medtronic – Consultant. Pentax Medical – Consultant, Grant/Research Support.
Srinivas Gaddam: Boston Scientific – Advisory Committee/Board Member.
Amrit Kamboj: Castle Biosciences – Consultant.
Anila Vasireddy, MD1, Apoorva K. Chandar, MBBS, MPH2, Mart Andrew Maravillas, MS3, Jaime A. Perez, PhD4, Sandra Algarin Perneth, MD5, Cadman Leggett, MD5, Prasad G. Iyer, MD, MS, FACG6, Srinivas Gaddam, MD, MPH7, Amrit K.. Kamboj, MD7, 39, Incidence of Young-Onset Barrett’s Esophagus is Increasing: A Population-Based Study From a Multi-Institutional National Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

