Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3B - Obesity / Biliary-Pancreas
49 - Artificial Intelligence-Assisted Digital Cholangioscopy for the Diagnosis and Morphological Characterization of Indeterminate Biliary Strictures: A Multicentric Study
Tuesday, October 29, 2024
2:45 PM - 2:55 PM ET
Location: Terrace Ballroom 2-3

Miguel Mascarenhas, MD, PhD
Centro Hospitalar Universitário de São João
Porto, Porto, Portugal
Presenting Author(s)
Miguel Mascarenhas, MD, PhD1, Jessica Widmer, MD2, Mariano González-Haba, MD3, Francisco Mendes, MD1, Tamas Gonda, MD4, Belen Agudo, MD3, Tiago Ribeiro, MD1, Miguel Martins, MD1, Antonio Pinto da Costa, MD5, Yousef Fazel, MD2, Marcos Eduardo Lera dos Santos, MD, PhD6, Eduardo Horneaux de Moura, MD, PhD6, Filipe Vilas Boas, MD, PhD7, Pedro Pereira, MD, PhD1, Bruno Mendes, 8, João Ferreira, PhD8, Guilherme Macedo, MD, PhD, FACG1
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2NYU Langone Health, New York, NY; 3Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Madrid, Spain; 4New York University Langone Health, New York, NY; 5Hospital Universitario Puerta de Hierro-Majadahonda, Madrid, Madrid, Spain; 6Hospital das Clínicas da Faculdade de Medicina da Universidade de Sao Paulo, São Paulo, Sao Paulo, Brazil; 7Centro Hospitalar Universitário São João, Porto, Porto, Portugal; 8Faculdade de Engenharia da Universidade do Porto, Porto, Porto, Portugal
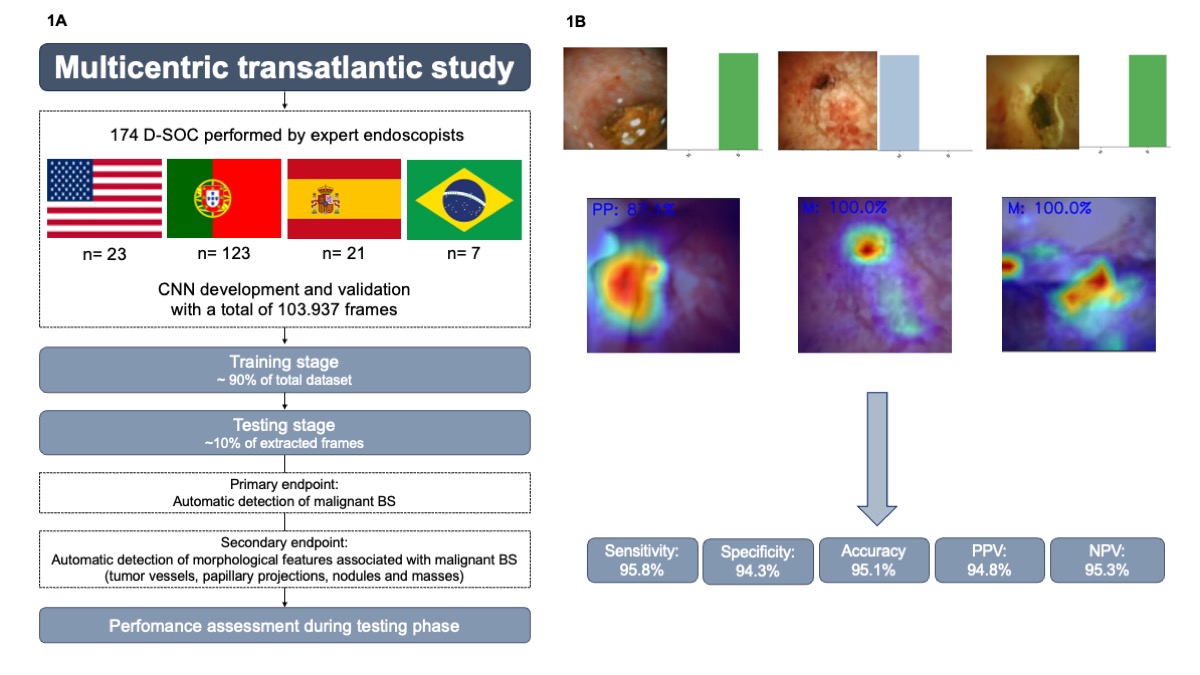
Introduction: The diagnostic workup of indeterminate biliary strictures often involves multiple exams, with suboptimal diagnostic accuracy. Artificial intelligence (AI) applied to digital single-operator cholangioscopy (D-SOC) is expected to enhance the diagnostic yield of indeterminate biliary strictures. In fact, data from previous studies suggest the potential of AI-powered D-SOC for early and more accurate detection of malignant biliary strictures. This multicentric study aims to validate a convolutional neural network (CNN) for automatic detection and morphological characterization of malignant biliary strictures.
Methods: A total of 174 D-SOC exams from 4 high volume centers (Portugal, Spain, the United States of America and Brazil) were used for development of the model. Each frame was classified as normal / benign finding or as a malignant lesion according to available histopathological analysis. Additionally, our group evaluated the CNN performance for detecting morphological features suggestive of malignant biliary strictures, namely papillary projections, tumor vessels and nodules. The image dataset was split in a training and validation dataset with a 90/10% ratio. The testing dataset was used for evaluating CNN performance, according to its sensitivity, specificity, accuracy, positive and negative predictive values (PPV and NPV, respectively) and area under the receiver-operating characteristic curve.
Results: A total of 103 937 images were included (54 196 malignant and 49 741 of benign findings). The model had an overall accuracy of 95.1% for detecting malignant biliary strictures, with 95.8% sensitivity and 94.3% specificity and a PPV and NPV of 94.8% and 95.3%, respectively. Additionally, the CNN identified papillary projections and tumor vessels with 89.2% and 73.9% accuracy, respectively.
Discussion: Our group developed a CNN capable of accurately detecting malignant biliary strictures in D-SOC procedures. This model was developed and validated in a large dataset from 4 distinct demographic contexts, reducing the impact of demographic bias. Artificial intelligence application to D-SOC has the potential to significantly augment the diagnostic yield of this exam, changing the clinical outcome of patients with suspected malignant biliary stricture.
Disclosures:
Miguel Mascarenhas, MD, PhD1, Jessica Widmer, MD2, Mariano González-Haba, MD3, Francisco Mendes, MD1, Tamas Gonda, MD4, Belen Agudo, MD3, Tiago Ribeiro, MD1, Miguel Martins, MD1, Antonio Pinto da Costa, MD5, Yousef Fazel, MD2, Marcos Eduardo Lera dos Santos, MD, PhD6, Eduardo Horneaux de Moura, MD, PhD6, Filipe Vilas Boas, MD, PhD7, Pedro Pereira, MD, PhD1, Bruno Mendes, 8, João Ferreira, PhD8, Guilherme Macedo, MD, PhD, FACG1, 49, Artificial Intelligence-Assisted Digital Cholangioscopy for the Diagnosis and Morphological Characterization of Indeterminate Biliary Strictures: A Multicentric Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2NYU Langone Health, New York, NY; 3Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Madrid, Spain; 4New York University Langone Health, New York, NY; 5Hospital Universitario Puerta de Hierro-Majadahonda, Madrid, Madrid, Spain; 6Hospital das Clínicas da Faculdade de Medicina da Universidade de Sao Paulo, São Paulo, Sao Paulo, Brazil; 7Centro Hospitalar Universitário São João, Porto, Porto, Portugal; 8Faculdade de Engenharia da Universidade do Porto, Porto, Porto, Portugal
Introduction: The diagnostic workup of indeterminate biliary strictures often involves multiple exams, with suboptimal diagnostic accuracy. Artificial intelligence (AI) applied to digital single-operator cholangioscopy (D-SOC) is expected to enhance the diagnostic yield of indeterminate biliary strictures. In fact, data from previous studies suggest the potential of AI-powered D-SOC for early and more accurate detection of malignant biliary strictures. This multicentric study aims to validate a convolutional neural network (CNN) for automatic detection and morphological characterization of malignant biliary strictures.
Methods: A total of 174 D-SOC exams from 4 high volume centers (Portugal, Spain, the United States of America and Brazil) were used for development of the model. Each frame was classified as normal / benign finding or as a malignant lesion according to available histopathological analysis. Additionally, our group evaluated the CNN performance for detecting morphological features suggestive of malignant biliary strictures, namely papillary projections, tumor vessels and nodules. The image dataset was split in a training and validation dataset with a 90/10% ratio. The testing dataset was used for evaluating CNN performance, according to its sensitivity, specificity, accuracy, positive and negative predictive values (PPV and NPV, respectively) and area under the receiver-operating characteristic curve.
Results: A total of 103 937 images were included (54 196 malignant and 49 741 of benign findings). The model had an overall accuracy of 95.1% for detecting malignant biliary strictures, with 95.8% sensitivity and 94.3% specificity and a PPV and NPV of 94.8% and 95.3%, respectively. Additionally, the CNN identified papillary projections and tumor vessels with 89.2% and 73.9% accuracy, respectively.
Discussion: Our group developed a CNN capable of accurately detecting malignant biliary strictures in D-SOC procedures. This model was developed and validated in a large dataset from 4 distinct demographic contexts, reducing the impact of demographic bias. Artificial intelligence application to D-SOC has the potential to significantly augment the diagnostic yield of this exam, changing the clinical outcome of patients with suspected malignant biliary stricture.
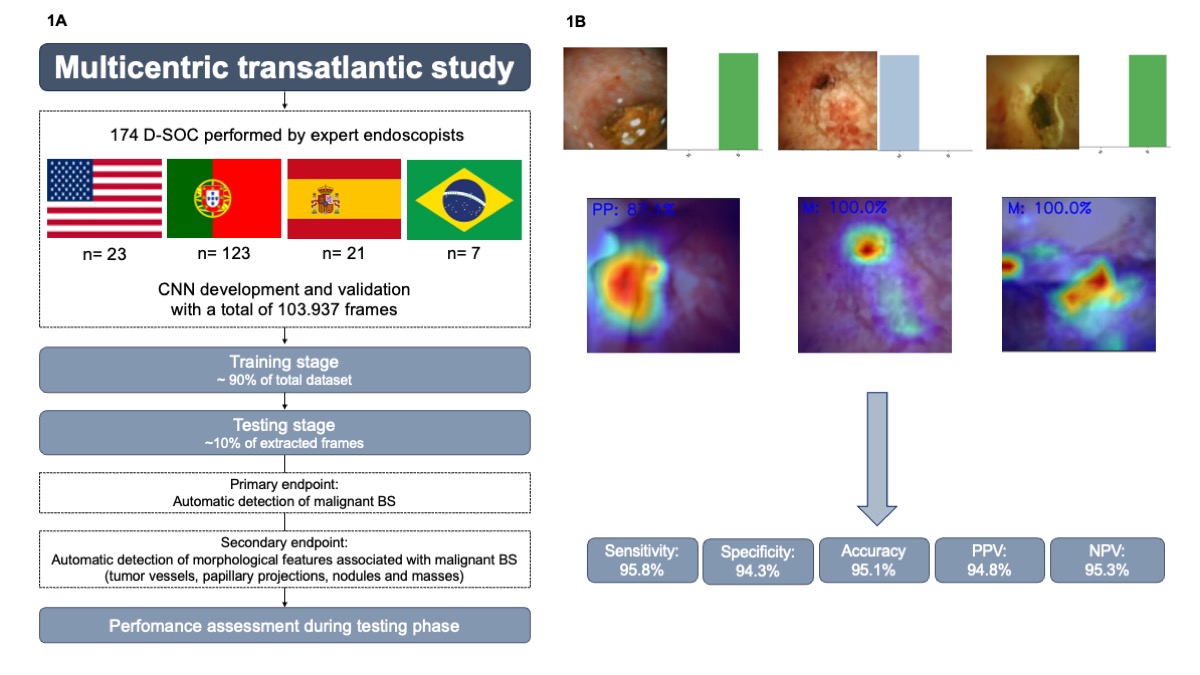
Figure: Figure 1 - Artificial Intelligence-Assisted Digital Cholangioscopy for the Diagnosis and Morphological Characterization of Indeterminate Biliary Strictures: A Multicentric Study. 1A - Study Design. 1B – Example of Convolutional Neural Network Output and Heatmaps. Performance Measures of the CNN for detection of malignant biliary strictures. D-SOC – Digital Single-Operator Cholangioscopy; CNN – Convolutional Neural Network; BS – biliary stricture; M – malign; B – benign; PPV – positive predictive value; NPV – negative predictive value.
Disclosures:
Miguel Mascarenhas indicated no relevant financial relationships.
Jessica Widmer indicated no relevant financial relationships.
Mariano González-Haba indicated no relevant financial relationships.
Francisco Mendes indicated no relevant financial relationships.
Tamas Gonda indicated no relevant financial relationships.
Belen Agudo indicated no relevant financial relationships.
Tiago Ribeiro indicated no relevant financial relationships.
Miguel Martins indicated no relevant financial relationships.
Antonio Pinto da Costa indicated no relevant financial relationships.
Yousef Fazel indicated no relevant financial relationships.
Marcos Eduardo Lera dos Santos indicated no relevant financial relationships.
Eduardo Horneaux de Moura indicated no relevant financial relationships.
Filipe Vilas Boas indicated no relevant financial relationships.
Pedro Pereira indicated no relevant financial relationships.
Bruno Mendes indicated no relevant financial relationships.
João Ferreira indicated no relevant financial relationships.
Guilherme Macedo indicated no relevant financial relationships.
Miguel Mascarenhas, MD, PhD1, Jessica Widmer, MD2, Mariano González-Haba, MD3, Francisco Mendes, MD1, Tamas Gonda, MD4, Belen Agudo, MD3, Tiago Ribeiro, MD1, Miguel Martins, MD1, Antonio Pinto da Costa, MD5, Yousef Fazel, MD2, Marcos Eduardo Lera dos Santos, MD, PhD6, Eduardo Horneaux de Moura, MD, PhD6, Filipe Vilas Boas, MD, PhD7, Pedro Pereira, MD, PhD1, Bruno Mendes, 8, João Ferreira, PhD8, Guilherme Macedo, MD, PhD, FACG1, 49, Artificial Intelligence-Assisted Digital Cholangioscopy for the Diagnosis and Morphological Characterization of Indeterminate Biliary Strictures: A Multicentric Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


