Oral Paper Presentation
Annual Scientific Meeting
Session: Presidential Plenary Session 1
3 - Insurance Coverage for Endoscopic Bariatric Therapy in 2024: Analyses of the Top Insurers in the U.S.
Monday, October 28, 2024
8:24 AM - 8:36 AM ET
Location: Terrace Ballroom
.jpg)
Sagar Shah, MD
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Cynthia Okafor, BS1, Dima Bechenati, MD2, Sagar Shah, MD3, Danny Issa, MD3
1University of Texas Medical Branch, Galveston, TX; 2Mayo Clinic, Rochester, MN; 3David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Endoscopic bariatric therapy (EBT) is recognized as a safe and effective treatment for obesity and related conditions. However, variable and outdated insurance coverage criteria pose a significant barrier, leading to inequities in patient care and impacting both health outcomes and healthcare providers' decisions. To identify common patterns in insurance coverage for adults considering EBT, we analyzed policies for different procedures among top U.S. insurers.
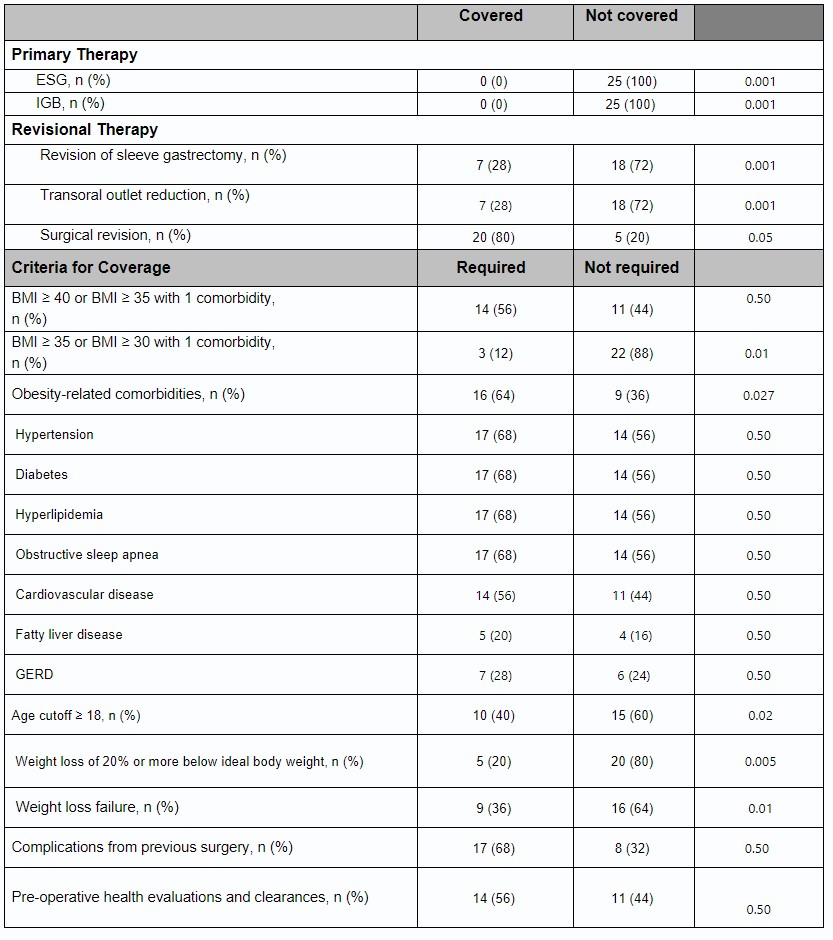
Methods: We reviewed current coverage policies of the 25 top U.S. health insurance companies from the National Association of Insurance Commissioners, focusing on coverage and requirements for 4 EBT procedures: primary therapies {endoscopic sleeve gastroplasty (ESG) and intragastric balloon (IGB)} and revisional therapies {transoral outlet reduction (TORe) and sleeve gastrectomy revision}. Analyzed criteria included BMI thresholds, preoperative medical and mental health evaluations, age restrictions, documented surgical complications, and presence of obesity-related comorbidities. Data were obtained through publicly available policy documents and telephone calls to customer services online policy was unavailable. This study was supported by the ACG Scholarship Award for medical students from under-represented minorities.
Results: Twenty-three (92%) insurers had clear coverage policies online for EBT. None of the 25 insurers included primary EBT in their coverage, while 20(80%) covered revisional EBT (P < 0.001). All policies cited criteria for revisional therapies. Diabetes mellitus, hypertension, and obstructive sleep apnea were equally cited as comorbidities for inclusion in revision therapies (n=17, 68%). Other comorbidities included cardiovascular disease (n=14, 56%), hyperlipidemia (n=9, 36%), gastroesophageal reflux disease (n=7, 28%), arthropathy (n=7, 28%), and fatty liver disease (n=5, 20%). Complications from primary surgery were criteria for 17(68%) insurers. Some insurers also required pre-operative health evaluations and clearances by multidisciplinary teams (n=14, 56%).
Discussion: None of the top 25 health insurance providers in the U.S. have current policies covering primary endoscopic bariatric therapy. Conversely, the majority cover revisional therapies when criteria are met. This study calls for standardized and updated coverage for EBT that matches available evidence. With the increasing prevalence of obesity, overcoming the insurance barrier is crucial to improving patient access and outcomes of new treatments.
Disclosures:
Cynthia Okafor, BS1, Dima Bechenati, MD2, Sagar Shah, MD3, Danny Issa, MD3, 3, Insurance Coverage for Endoscopic Bariatric Therapy in 2024: Analyses of the Top Insurers in the U.S., ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2Mayo Clinic, Rochester, MN; 3David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Endoscopic bariatric therapy (EBT) is recognized as a safe and effective treatment for obesity and related conditions. However, variable and outdated insurance coverage criteria pose a significant barrier, leading to inequities in patient care and impacting both health outcomes and healthcare providers' decisions. To identify common patterns in insurance coverage for adults considering EBT, we analyzed policies for different procedures among top U.S. insurers.
Methods: We reviewed current coverage policies of the 25 top U.S. health insurance companies from the National Association of Insurance Commissioners, focusing on coverage and requirements for 4 EBT procedures: primary therapies {endoscopic sleeve gastroplasty (ESG) and intragastric balloon (IGB)} and revisional therapies {transoral outlet reduction (TORe) and sleeve gastrectomy revision}. Analyzed criteria included BMI thresholds, preoperative medical and mental health evaluations, age restrictions, documented surgical complications, and presence of obesity-related comorbidities. Data were obtained through publicly available policy documents and telephone calls to customer services online policy was unavailable. This study was supported by the ACG Scholarship Award for medical students from under-represented minorities.
Results: Twenty-three (92%) insurers had clear coverage policies online for EBT. None of the 25 insurers included primary EBT in their coverage, while 20(80%) covered revisional EBT (P < 0.001). All policies cited criteria for revisional therapies. Diabetes mellitus, hypertension, and obstructive sleep apnea were equally cited as comorbidities for inclusion in revision therapies (n=17, 68%). Other comorbidities included cardiovascular disease (n=14, 56%), hyperlipidemia (n=9, 36%), gastroesophageal reflux disease (n=7, 28%), arthropathy (n=7, 28%), and fatty liver disease (n=5, 20%). Complications from primary surgery were criteria for 17(68%) insurers. Some insurers also required pre-operative health evaluations and clearances by multidisciplinary teams (n=14, 56%).
Discussion: None of the top 25 health insurance providers in the U.S. have current policies covering primary endoscopic bariatric therapy. Conversely, the majority cover revisional therapies when criteria are met. This study calls for standardized and updated coverage for EBT that matches available evidence. With the increasing prevalence of obesity, overcoming the insurance barrier is crucial to improving patient access and outcomes of new treatments.
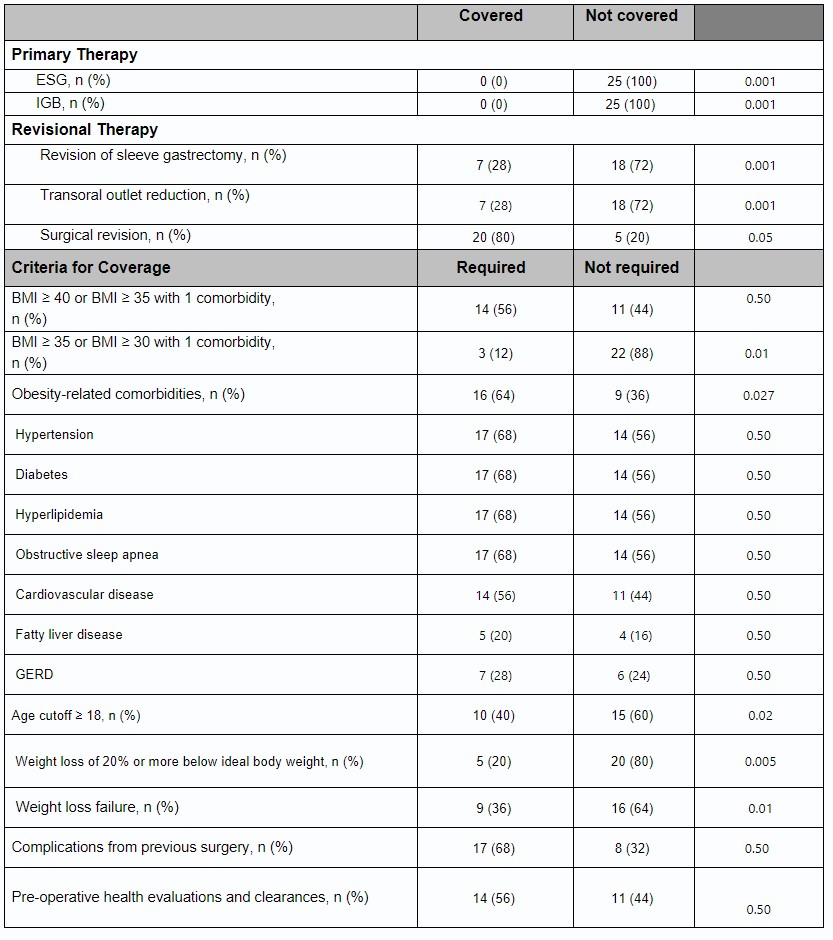
Table: Table 1: Frequency of coverage for primary and secondary bariatric therapy and documented requirements for covering revisional therapy among the top 25 insurers. Weight loss failure defined as: losing less than 50% of excess weight or not reaching within 30% of ideal body weight.
Disclosures:
Cynthia Okafor indicated no relevant financial relationships.
Dima Bechenati indicated no relevant financial relationships.
Sagar Shah indicated no relevant financial relationships.
Danny Issa: Boston Scientific – Consultant, Speakers Bureau. Eli Lilly – Speakers Bureau.
Cynthia Okafor, BS1, Dima Bechenati, MD2, Sagar Shah, MD3, Danny Issa, MD3, 3, Insurance Coverage for Endoscopic Bariatric Therapy in 2024: Analyses of the Top Insurers in the U.S., ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


