Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2B - Colon / General Endoscopy / GI Bleed / Practice Management
30 - Risk of Bleeding After Colorectal Endoscopic Mucosal Resection in Patients With Cirrhosis: A Propensity-Matched Analysis of the US Collaborative Network
Tuesday, October 29, 2024
8:50 AM - 9:00 AM ET
Location: Terrace Ballroom 2-3

Azizullah Beran, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Award: ACG Outstanding Research Award in the Colon Category (Trainee)
Azizullah Beran, MD1, Khaled Elfert, MD2, Mouhand F.H. Mohamed, MD, MSc3, Douglas Rex, MD1, Indira Bhavsar-Burke, MD, MHPE4, John Guardiola, MD1
1Indiana University School of Medicine, Indianapolis, IN; 2West Virginia University, Morgantown, WV; 3Mayo Clinic, Rochester, MN; 4University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Endoscopic mucosal resection (EMR) is the preferred treatment for large nonpedunculated colorectal polyps. Gastrointestinal (GI) bleeding is the most frequent major adverse event after colorectal EMR. Patients with cirrhosis may bleed because of coagulation factor synthesis disruption, thrombocytopenia, or portal hypertension.Risk of bleeding following colorectal EMR in patients with cirrhosis has not been evaluated. We conducted a retrospective U.S.-based, propensity-matched cohort study to assess risk of post-colorectal EMR bleeding in patients with cirrhosis.
Methods: We analyzed the U.S. Collaborative Network in the TriNetX platform through 4/6/2024 for patients with cirrhosis who underwent colorectal EMR. One-to-one propensity score matching was performed. The risk of each outcome was calculated and expressed as odds ratio (OR) with a 95% confidence interval (CI). Two-sided p-value < 0.05 was considered statistically significant. Primary outcome was risk of lower GI bleeding within 30 days of EMR. Secondary outcomes were endoscopic reintervention for control of bleeding, emergency department (ED) visits, inpatient admissions, and intensive care unit (ICU) admissions.
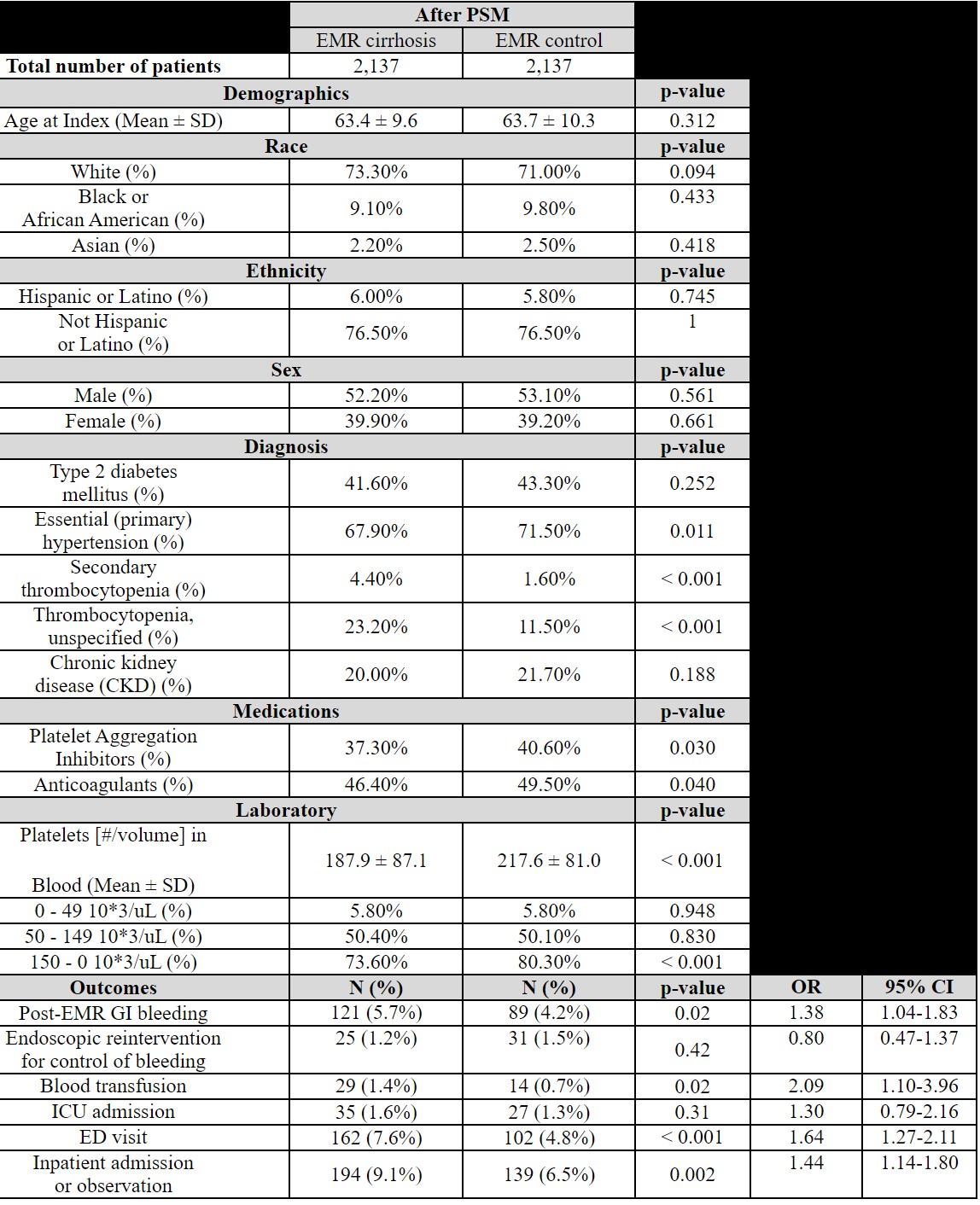
Results: After one-to-one propensity score matching for age, race, ethnicity, sex, hypertension, diabetes mellitus, chronic kidney disease, thrombocytopenia, use of anticoagulants/antiplatelets, there were 4,274 subjects (2,137 in the cirrhosis cohort and 2,137 in the matched control cohort) who underwent colorectal EMR. Patients with cirrhosis had an increased risk of post-EMR bleeding compared with matched control subjects (OR 1.38, 95% CI 1.04-1.83, p=0.02) along with increased blood transfusions (OR 2.09, 95% CI 1.10-3.96, p=0.02), ED visits (OR 1.64, 95% CI 1.27-2.11, p< 0.001) and inpatient admissions (OR 1.44, 95% CI 1.14-1.80, p=0.002), but no differences in endoscopic reinterventions for control of bleeding (OR 0.80, 95% CI 0.47-1.37, p=0.42) and ICU admission (OR 1.30, 95% CI 0.79-2.16, p=0.31). (Table)
Discussion: Patients with cirrhosis have a higher risk of post-EMR bleeding and require more blood transfusions compared to matched controls, but absolute risk remains low. The rates of endoscopic reintervention for bleeding and ICU admissions are similar between the groups. Optimizing patients with cirrhosis prior to colorectal EMR and monitoring for post-procedure bleeding remains important. Conservative, supportive management of bleeding in cirrhotic patients may be as effective as in non-cirrhotic patients.
Disclosures:
Azizullah Beran, MD1, Khaled Elfert, MD2, Mouhand F.H. Mohamed, MD, MSc3, Douglas Rex, MD1, Indira Bhavsar-Burke, MD, MHPE4, John Guardiola, MD1, 30, Risk of Bleeding After Colorectal Endoscopic Mucosal Resection in Patients With Cirrhosis: A Propensity-Matched Analysis of the US Collaborative Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Azizullah Beran, MD1, Khaled Elfert, MD2, Mouhand F.H. Mohamed, MD, MSc3, Douglas Rex, MD1, Indira Bhavsar-Burke, MD, MHPE4, John Guardiola, MD1
1Indiana University School of Medicine, Indianapolis, IN; 2West Virginia University, Morgantown, WV; 3Mayo Clinic, Rochester, MN; 4University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Endoscopic mucosal resection (EMR) is the preferred treatment for large nonpedunculated colorectal polyps. Gastrointestinal (GI) bleeding is the most frequent major adverse event after colorectal EMR. Patients with cirrhosis may bleed because of coagulation factor synthesis disruption, thrombocytopenia, or portal hypertension.Risk of bleeding following colorectal EMR in patients with cirrhosis has not been evaluated. We conducted a retrospective U.S.-based, propensity-matched cohort study to assess risk of post-colorectal EMR bleeding in patients with cirrhosis.
Methods: We analyzed the U.S. Collaborative Network in the TriNetX platform through 4/6/2024 for patients with cirrhosis who underwent colorectal EMR. One-to-one propensity score matching was performed. The risk of each outcome was calculated and expressed as odds ratio (OR) with a 95% confidence interval (CI). Two-sided p-value < 0.05 was considered statistically significant. Primary outcome was risk of lower GI bleeding within 30 days of EMR. Secondary outcomes were endoscopic reintervention for control of bleeding, emergency department (ED) visits, inpatient admissions, and intensive care unit (ICU) admissions.
Results: After one-to-one propensity score matching for age, race, ethnicity, sex, hypertension, diabetes mellitus, chronic kidney disease, thrombocytopenia, use of anticoagulants/antiplatelets, there were 4,274 subjects (2,137 in the cirrhosis cohort and 2,137 in the matched control cohort) who underwent colorectal EMR. Patients with cirrhosis had an increased risk of post-EMR bleeding compared with matched control subjects (OR 1.38, 95% CI 1.04-1.83, p=0.02) along with increased blood transfusions (OR 2.09, 95% CI 1.10-3.96, p=0.02), ED visits (OR 1.64, 95% CI 1.27-2.11, p< 0.001) and inpatient admissions (OR 1.44, 95% CI 1.14-1.80, p=0.002), but no differences in endoscopic reinterventions for control of bleeding (OR 0.80, 95% CI 0.47-1.37, p=0.42) and ICU admission (OR 1.30, 95% CI 0.79-2.16, p=0.31). (Table)
Discussion: Patients with cirrhosis have a higher risk of post-EMR bleeding and require more blood transfusions compared to matched controls, but absolute risk remains low. The rates of endoscopic reintervention for bleeding and ICU admissions are similar between the groups. Optimizing patients with cirrhosis prior to colorectal EMR and monitoring for post-procedure bleeding remains important. Conservative, supportive management of bleeding in cirrhotic patients may be as effective as in non-cirrhotic patients.
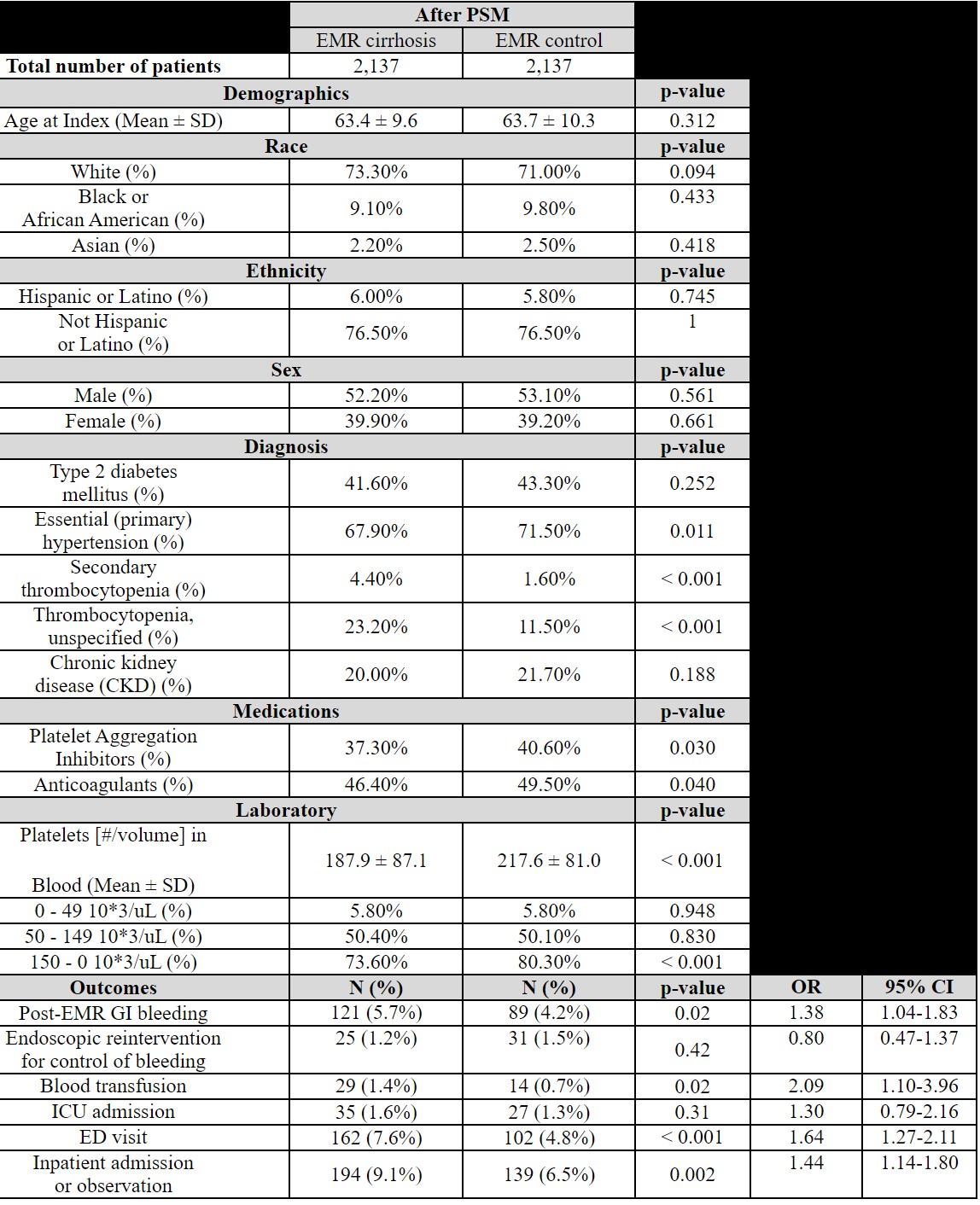
Table: Abbreviations: CI: confidence interval, ED: emergency department, EMR: endoscopic mucosal resection, GI: gastrointestinal, ICU: intensive care unit, OR: odds ratio.
Disclosures:
Azizullah Beran indicated no relevant financial relationships.
Khaled Elfert indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
Douglas Rex: Acacia Pharmaceuticals – Consultant. Boston Scientific – Consultant. Braintree Laboratories – Consultant, Grant/Research Support. Erbe USA – Grant/Research Support. Medivators – Grant/Research Support. Medtronic – Consultant. Norgine – Consultant. Olympus Corporation – Consultant, Grant/Research Support. Satisfai Health – Stock Options.
Indira Bhavsar-Burke indicated no relevant financial relationships.
John Guardiola: Boston Scientific Corporation – Travel Support. Olympus Corporation – Travel Support.
Azizullah Beran, MD1, Khaled Elfert, MD2, Mouhand F.H. Mohamed, MD, MSc3, Douglas Rex, MD1, Indira Bhavsar-Burke, MD, MHPE4, John Guardiola, MD1, 30, Risk of Bleeding After Colorectal Endoscopic Mucosal Resection in Patients With Cirrhosis: A Propensity-Matched Analysis of the US Collaborative Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.



