Monday Poster Session
Category: Biliary/Pancreas
P1829 - Pancreatic Neuroendocrine Tumor Mimicking Cystadenoma in a Young Female
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mark DeSantis, DO, MS (he/him/his)
AtlantiCare Regional Medical Center
Brigantine, NJ
Presenting Author(s)
Mark DeSantis, DO, MS1, Debashis Reja, MD2, Sushil Ahlawat, MD, MS, MBBS2
1AtlantiCare Regional Medical Center, Atlantic City, NJ; 2SUNY Downstate Health Sciences University, Brooklyn, NY
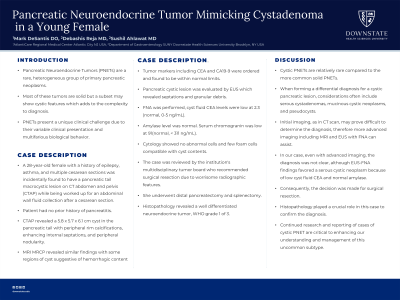
Introduction: Pancreatic Neuroendocrine Tumors (PNETs) are a rare, heterogeneous group of primary pancreatic neoplasms. Most of these tumors are solid but a subset may show cystic features which adds to the complexity to diagnosis. PNETs present a unique clinical challenge due to their variable clinical presentation and multifarious biological behavior.
Case Description/Methods: A 28-year-old female with a history of epilepsy, asthma, and multiple cesarean sections was incidentally found to have a pancreatic tail macrocystic lesion on CT abdomen and pelvis (CTAP) while being worked up for an abdominal wall fluid collection after a cesarean section. Patient had no prior history of pancreatitis. CTAP revealed a 5.8 x 5.7 x 6.1 cm cyst in the pancreatic tail with peripheral rim calcifications, enhancing internal septations, and peripheral nodularity. MRI MRCP revealed similar findings with some regions of cyst suggestive of hemorrhagic content. Tumor markers including CEA and CA19-9 were ordered and found to be within normal limits. Pancreatic cystic lesion was evaluated by EUS which revealed septations and granular debris. FNA was performed, cyst fluid CEA levels were low at 2.3 (normal, 0-5 ng/mL). Amylase level was normal. Serum chromogranin was low at 91(normal, < 311 ng/mL). Cytology showed no abnormal cells and few foam cells compatible with cyst contents. The case was reviewed by the institution's multidisciplinary tumor board who recommended surgical resection due to worrisome radiographic features. She underwent distal pancreatectomy and splenectomy. Histopathology revealed a well differentiated neuroendocrine tumor, WHO grade 1 of 3.
Discussion: Cystic PNETs are relatively rare compared to the more common solid PNETs. When forming a differential diagnosis for a cystic pancreatic lesion, considerations often include serous cystadenomas, mucinous cystic neoplasms, and pseudocysts. Initial imaging, as in CT scan, may prove difficult to determine the diagnosis, therefore more advanced imaging including MRI and EUS with FNA can assist. In our case, even with advanced imaging, the diagnosis was not clear, although EUS-FNA findings favored a serous cystic neoplasm because of low cyst fluid CEA and normal amylase. Consequently, the decision was made for surgical resection. Histopathology played a crucial role in this case to confirm the diagnosis. Continued research and reporting of cases of cystic PNET are critical to enhancing our understanding and management of this uncommon subtype.
Disclosures:
Mark DeSantis, DO, MS1, Debashis Reja, MD2, Sushil Ahlawat, MD, MS, MBBS2. P1829 - Pancreatic Neuroendocrine Tumor Mimicking Cystadenoma in a Young Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1AtlantiCare Regional Medical Center, Atlantic City, NJ; 2SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Pancreatic Neuroendocrine Tumors (PNETs) are a rare, heterogeneous group of primary pancreatic neoplasms. Most of these tumors are solid but a subset may show cystic features which adds to the complexity to diagnosis. PNETs present a unique clinical challenge due to their variable clinical presentation and multifarious biological behavior.
Case Description/Methods: A 28-year-old female with a history of epilepsy, asthma, and multiple cesarean sections was incidentally found to have a pancreatic tail macrocystic lesion on CT abdomen and pelvis (CTAP) while being worked up for an abdominal wall fluid collection after a cesarean section. Patient had no prior history of pancreatitis. CTAP revealed a 5.8 x 5.7 x 6.1 cm cyst in the pancreatic tail with peripheral rim calcifications, enhancing internal septations, and peripheral nodularity. MRI MRCP revealed similar findings with some regions of cyst suggestive of hemorrhagic content. Tumor markers including CEA and CA19-9 were ordered and found to be within normal limits. Pancreatic cystic lesion was evaluated by EUS which revealed septations and granular debris. FNA was performed, cyst fluid CEA levels were low at 2.3 (normal, 0-5 ng/mL). Amylase level was normal. Serum chromogranin was low at 91(normal, < 311 ng/mL). Cytology showed no abnormal cells and few foam cells compatible with cyst contents. The case was reviewed by the institution's multidisciplinary tumor board who recommended surgical resection due to worrisome radiographic features. She underwent distal pancreatectomy and splenectomy. Histopathology revealed a well differentiated neuroendocrine tumor, WHO grade 1 of 3.
Discussion: Cystic PNETs are relatively rare compared to the more common solid PNETs. When forming a differential diagnosis for a cystic pancreatic lesion, considerations often include serous cystadenomas, mucinous cystic neoplasms, and pseudocysts. Initial imaging, as in CT scan, may prove difficult to determine the diagnosis, therefore more advanced imaging including MRI and EUS with FNA can assist. In our case, even with advanced imaging, the diagnosis was not clear, although EUS-FNA findings favored a serous cystic neoplasm because of low cyst fluid CEA and normal amylase. Consequently, the decision was made for surgical resection. Histopathology played a crucial role in this case to confirm the diagnosis. Continued research and reporting of cases of cystic PNET are critical to enhancing our understanding and management of this uncommon subtype.
Disclosures:
Mark DeSantis indicated no relevant financial relationships.
Debashis Reja indicated no relevant financial relationships.
Sushil Ahlawat indicated no relevant financial relationships.
Mark DeSantis, DO, MS1, Debashis Reja, MD2, Sushil Ahlawat, MD, MS, MBBS2. P1829 - Pancreatic Neuroendocrine Tumor Mimicking Cystadenoma in a Young Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
