Tuesday Poster Session
Category: GI Bleeding
P4244 - Rare Presentation of Isolated Gastric Varices Secondary to Chronic Splenic Artery Calcification
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- YD
Yogitha R. Dadi, MBBS (she/her/hers)
Southern Illinois University
Springfield, IL
Presenting Author(s)
Yogitha R. Dadi, MBBS1, Sophia Dar, MD1, Abdul Swied, MD2
1Southern Illinois University, Springfield, IL; 2Southern Illinois University School of Medicine, Springfield, IL
Introduction: Isolated Gastric Varices (IGV) are rare, often due to splenic vein thrombosis (SVT) from pancreatitis or neoplasms. We report a case of IGV1 (< 2% of all GV) due to chronic splenic artery calcification leading to splenic infarction and subsequent SVT.
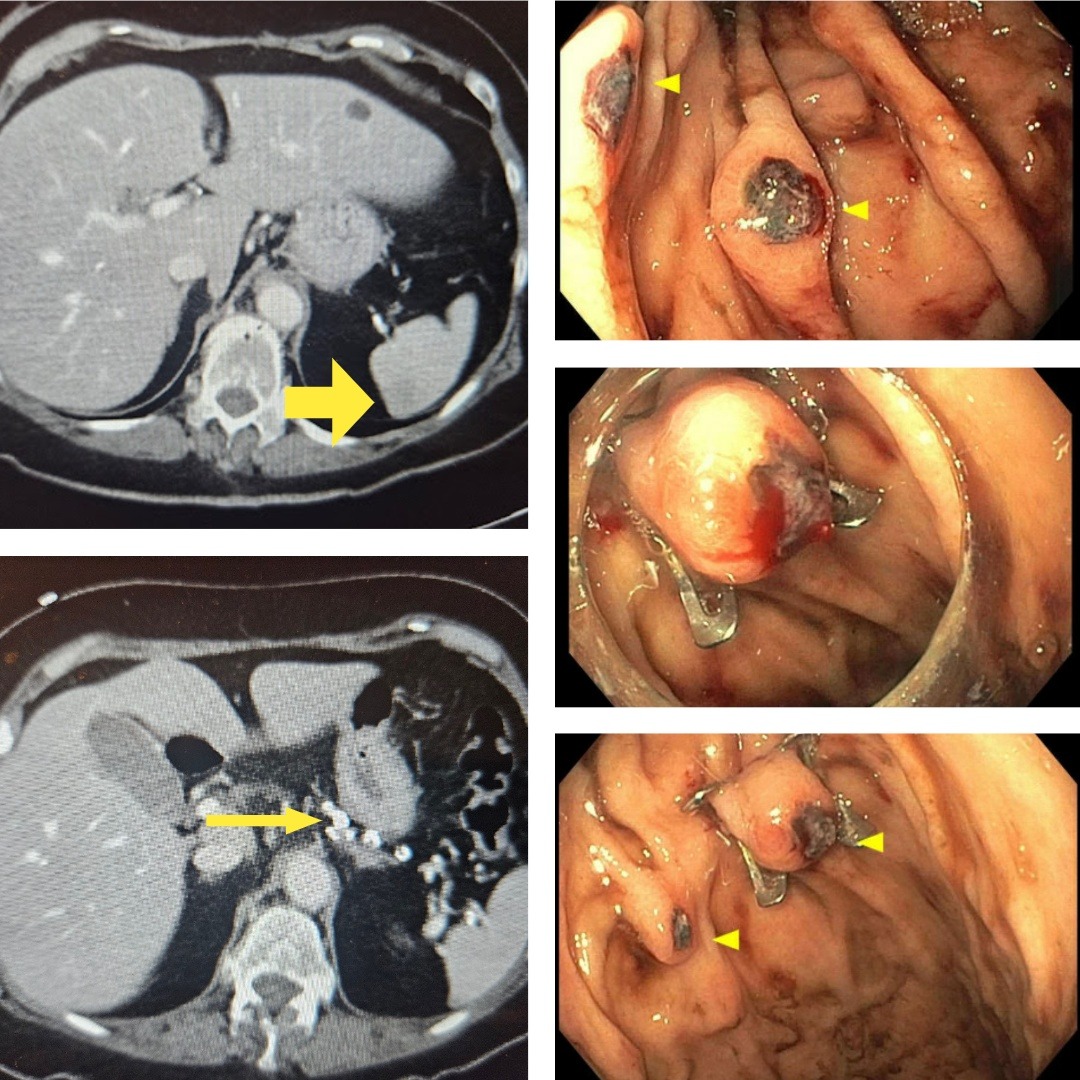
Case Description/Methods: A 77-year-old female with a medical history of diabetes, coronary artery disease, duodenal ulcers presented to the ER with nausea, weakness, fall, and multiple episodes of hematemesis beginning in the ambulance ride. The patient was found to have DKA and a left fibula fracture on arrival, leading to her admission. Initial CT abdomen read suspected splenic infarct without elaboration. Although there is no known history of pancreatitis or cirrhosis, given ongoing hematemesis and severe drop of hemoglobin from a baseline of 12 to 7.8 g/dL, the patient was taken emergently for EGD. Endoscopy revealed two lesions oozing blood in the fundus of the stomach, initially thought to be Dieulafoy lesions; one over-the-scope clip (OVESCO) was placed on the first lesion. Upon further inspection along the fundus, there was a concern for lesions to be IGV, as dilated vessels were observed. The second lesion was clipped with two through-the-scope clips. After the EGD, the initial CT imaging was reviewed with multiple radiologists who identified a highly tortuous and calcified splenic artery with nearly no flow causing the splenic infarction originally commented on, along with a large splenorenal shunt with multiple collaterals to the gastric fundus. We hypothesize that splenic artery abnormalities led to stasis, resulting in SVT and the subsequent development of IGV. BRTO or similar procedures were discussed but were not considered viable options due to difficult access. It would lead to back pressure, even if successful, worsening the varices. After a multidisciplinary discussion, it was decided that the best management would be splenectomy. The patient was scheduled for an elective splenectomy two weeks later to allow time for medical optimization.
Discussion: Splenectomy eliminates collateral venous flow and prevents future GV bleeding secondary to SVT. Elderly, diabetic populations often exhibit splenic artery abnormalities predisposing to SVT and IGV. This case underscores the need for a multidisciplinary approach in GI bleeding without typical risk factors. Further research is warranted to understand the pathophysiology of splenic artery abnormalities and their association with portal hypertension complications.
Disclosures:
Yogitha R. Dadi, MBBS1, Sophia Dar, MD1, Abdul Swied, MD2. P4244 - Rare Presentation of Isolated Gastric Varices Secondary to Chronic Splenic Artery Calcification, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Southern Illinois University, Springfield, IL; 2Southern Illinois University School of Medicine, Springfield, IL
Introduction: Isolated Gastric Varices (IGV) are rare, often due to splenic vein thrombosis (SVT) from pancreatitis or neoplasms. We report a case of IGV1 (< 2% of all GV) due to chronic splenic artery calcification leading to splenic infarction and subsequent SVT.
Case Description/Methods: A 77-year-old female with a medical history of diabetes, coronary artery disease, duodenal ulcers presented to the ER with nausea, weakness, fall, and multiple episodes of hematemesis beginning in the ambulance ride. The patient was found to have DKA and a left fibula fracture on arrival, leading to her admission. Initial CT abdomen read suspected splenic infarct without elaboration. Although there is no known history of pancreatitis or cirrhosis, given ongoing hematemesis and severe drop of hemoglobin from a baseline of 12 to 7.8 g/dL, the patient was taken emergently for EGD. Endoscopy revealed two lesions oozing blood in the fundus of the stomach, initially thought to be Dieulafoy lesions; one over-the-scope clip (OVESCO) was placed on the first lesion. Upon further inspection along the fundus, there was a concern for lesions to be IGV, as dilated vessels were observed. The second lesion was clipped with two through-the-scope clips. After the EGD, the initial CT imaging was reviewed with multiple radiologists who identified a highly tortuous and calcified splenic artery with nearly no flow causing the splenic infarction originally commented on, along with a large splenorenal shunt with multiple collaterals to the gastric fundus. We hypothesize that splenic artery abnormalities led to stasis, resulting in SVT and the subsequent development of IGV. BRTO or similar procedures were discussed but were not considered viable options due to difficult access. It would lead to back pressure, even if successful, worsening the varices. After a multidisciplinary discussion, it was decided that the best management would be splenectomy. The patient was scheduled for an elective splenectomy two weeks later to allow time for medical optimization.
Discussion: Splenectomy eliminates collateral venous flow and prevents future GV bleeding secondary to SVT. Elderly, diabetic populations often exhibit splenic artery abnormalities predisposing to SVT and IGV. This case underscores the need for a multidisciplinary approach in GI bleeding without typical risk factors. Further research is warranted to understand the pathophysiology of splenic artery abnormalities and their association with portal hypertension complications.
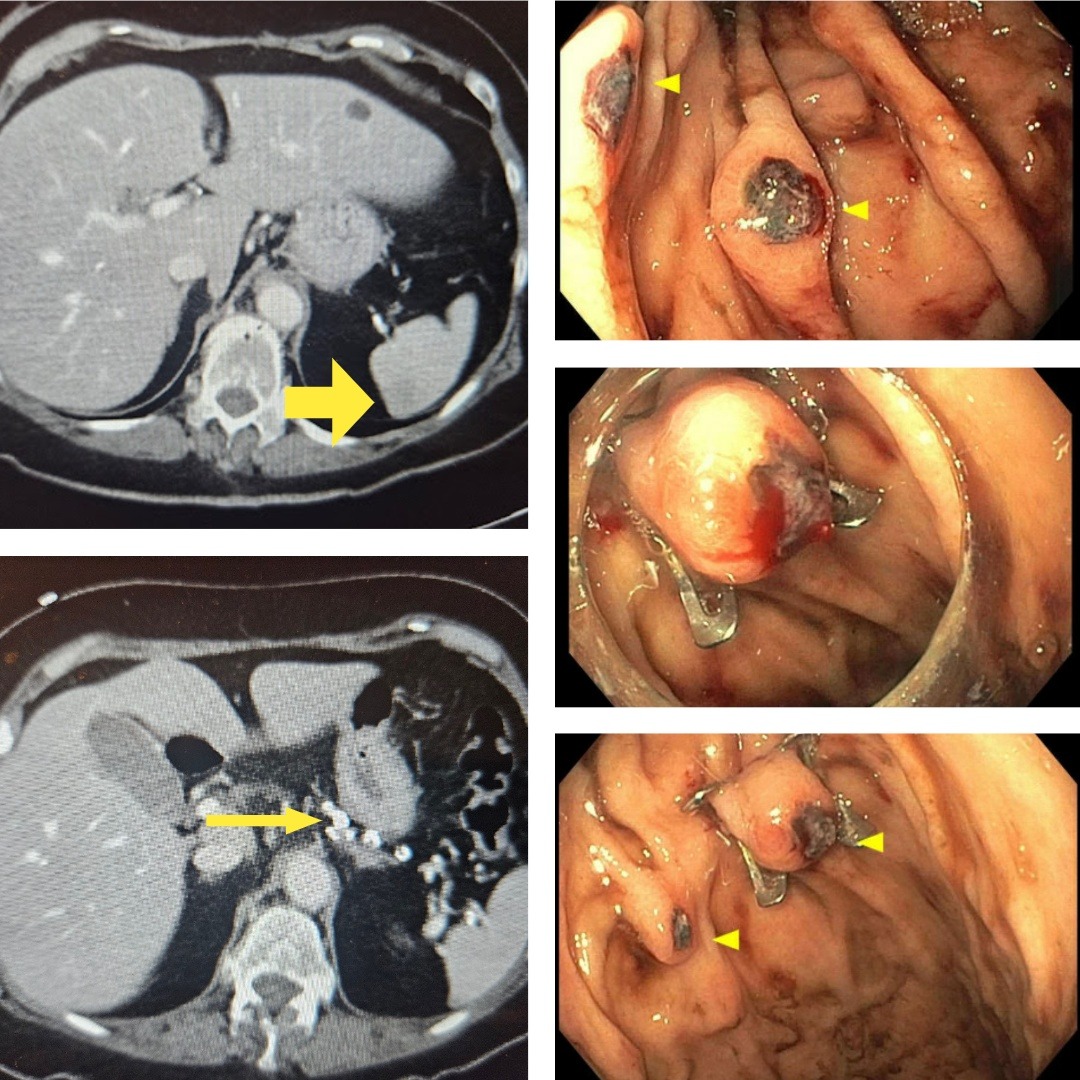
Figure: (Top Left) CT Abdomen with yellow arrow pointing to originally commented on splenic infarct. (Bottom Left) CT Abdomen with arrow displaying chronic splenic artery calcification. (Top Right) EGD imaging displaying IGV, originally thought to be Dieulafoy lesions. (Middle Right) Lesion with OVESCO clip placement. (Bottom Right) Another view of lesions after clip placement.
Disclosures:
Yogitha Dadi indicated no relevant financial relationships.
Sophia Dar indicated no relevant financial relationships.
Abdul Swied indicated no relevant financial relationships.
Yogitha R. Dadi, MBBS1, Sophia Dar, MD1, Abdul Swied, MD2. P4244 - Rare Presentation of Isolated Gastric Varices Secondary to Chronic Splenic Artery Calcification, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
