Tuesday Poster Session
Category: Liver
P4625 - Associations Between Liver Disease Etiology and Post-Liver Directed Treatment Mortality in HCC
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Chidi Iloabachie, BS
University of North Carolina at Chapel Hill School of Medicine
Carrboro, NC
Presenting Author(s)
Chidi Iloabachie, BS1, Yue Jiang, PhD2, Sydney Power, MD3, Arjun Juneja, BS4, Merete Lund, MD3, Gabe Lupu, MD3, Joyce Badal, MD4, David Seligson, MS5, Hanna Sanoff, MD3, David Mauro, MD3, David Gerber, MD4, Ted Yanagihara, MD3, Alfred S. Barritt, MD, MSCR6, Andrew Moon, MD, MPH3
1University of North Carolina at Chapel Hill School of Medicine, Carrboro, NC; 2Duke University, Chapel Hill, NC; 3University of North Carolina, Chapel Hill, NC; 4University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 5Center for Gastrointestinal Biology and Disease, University of North Carolina, Chapel Hill, NC; 6UNC, Chapel Hill, NC
Introduction: Hepatocellular carcinoma (HCC) is the most common cancer in patients with chronic liver disease and cirrhosis. Most patients with HCC receive one or more locoregional therapies (thermal ablation, transarterial chemo- or radioembolization, external beam radiation). The underlying liver diseases leading to HCC are changing rapidly with the advent of effective medications for hepatitis C virus (HCV) and hepatitis B virus (HBV) and the rising burden of obesity, diabetes, and unhealthy alcohol use. The degree to which liver disease etiology influences outcomes after locoregional therapies for HCC is uncertain. This study aimed to assess if the etiology of HCC is associated with mortality post-liver-directed therapy.
Methods: We performed a single-center retrospective analysis of adults with HCC treated with liver-directed locoregional therapies from 4/4/2014 to 12/31/2021. Baseline sociodemographic and clinical characteristics were extracted. The primary outcome was time to death after initial treatment. Etiologies of HCC were categorized as alcohol-associated (ALD), metabolic dysfunction-associated (MASLD), viral (HBV/HCV), and other. Patients with contributions from more than one of these categories were classified as multiple. Mortality was determined via linkage to state death databases with confirmation by chart review. We performed unadjusted and multivariable proportional hazards regression to assess potential associations between etiology and mortality, adjusting for potential confounders.
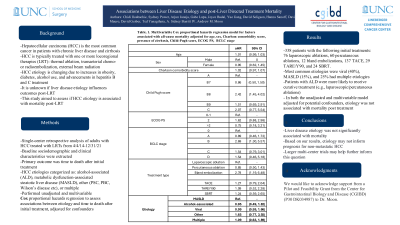
Results: This study included 338 patients with HCC with the following initial treatments: 76 laparoscopic ablations, 60 percutaneous ablations, 12 bland embolizations, 137 TACE, 29 TARE/Y90, and 24 SBRT. The most common etiologies among patients with only a single etiology were viral (N = 134; 40%) and MASLD (N = 52; 15%). 86 patients had multiple etiologies (25%). Patients with alcohol-associated etiology were more likely to receive curative treatment. In both the unadjusted and multivariable model adjusting for age, sex, Charlson comorbidity score, Child-Pugh score, ECOG PS, BCLC stage, and treatment type, we did not find an association between etiology and mortality post-treatment.
Discussion: In this retrospective study, liver disease etiology was not significantly associated with mortality. While larger multicenter trials may help further inform this question, data from this study suggests that etiology may not inform prognosis for non-metastatic HCC.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Chidi Iloabachie, BS1, Yue Jiang, PhD2, Sydney Power, MD3, Arjun Juneja, BS4, Merete Lund, MD3, Gabe Lupu, MD3, Joyce Badal, MD4, David Seligson, MS5, Hanna Sanoff, MD3, David Mauro, MD3, David Gerber, MD4, Ted Yanagihara, MD3, Alfred S. Barritt, MD, MSCR6, Andrew Moon, MD, MPH3. P4625 - Associations Between Liver Disease Etiology and Post-Liver Directed Treatment Mortality in HCC, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Carolina at Chapel Hill School of Medicine, Carrboro, NC; 2Duke University, Chapel Hill, NC; 3University of North Carolina, Chapel Hill, NC; 4University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 5Center for Gastrointestinal Biology and Disease, University of North Carolina, Chapel Hill, NC; 6UNC, Chapel Hill, NC
Introduction: Hepatocellular carcinoma (HCC) is the most common cancer in patients with chronic liver disease and cirrhosis. Most patients with HCC receive one or more locoregional therapies (thermal ablation, transarterial chemo- or radioembolization, external beam radiation). The underlying liver diseases leading to HCC are changing rapidly with the advent of effective medications for hepatitis C virus (HCV) and hepatitis B virus (HBV) and the rising burden of obesity, diabetes, and unhealthy alcohol use. The degree to which liver disease etiology influences outcomes after locoregional therapies for HCC is uncertain. This study aimed to assess if the etiology of HCC is associated with mortality post-liver-directed therapy.
Methods: We performed a single-center retrospective analysis of adults with HCC treated with liver-directed locoregional therapies from 4/4/2014 to 12/31/2021. Baseline sociodemographic and clinical characteristics were extracted. The primary outcome was time to death after initial treatment. Etiologies of HCC were categorized as alcohol-associated (ALD), metabolic dysfunction-associated (MASLD), viral (HBV/HCV), and other. Patients with contributions from more than one of these categories were classified as multiple. Mortality was determined via linkage to state death databases with confirmation by chart review. We performed unadjusted and multivariable proportional hazards regression to assess potential associations between etiology and mortality, adjusting for potential confounders.
Results: This study included 338 patients with HCC with the following initial treatments: 76 laparoscopic ablations, 60 percutaneous ablations, 12 bland embolizations, 137 TACE, 29 TARE/Y90, and 24 SBRT. The most common etiologies among patients with only a single etiology were viral (N = 134; 40%) and MASLD (N = 52; 15%). 86 patients had multiple etiologies (25%). Patients with alcohol-associated etiology were more likely to receive curative treatment. In both the unadjusted and multivariable model adjusting for age, sex, Charlson comorbidity score, Child-Pugh score, ECOG PS, BCLC stage, and treatment type, we did not find an association between etiology and mortality post-treatment.
Discussion: In this retrospective study, liver disease etiology was not significantly associated with mortality. While larger multicenter trials may help further inform this question, data from this study suggests that etiology may not inform prognosis for non-metastatic HCC.

Figure: Kaplan-Meier plot showing survival probability from time after first LRT treatment stratified by etiology
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Chidi Iloabachie indicated no relevant financial relationships.
Yue Jiang indicated no relevant financial relationships.
Sydney Power indicated no relevant financial relationships.
Arjun Juneja indicated no relevant financial relationships.
Merete Lund indicated no relevant financial relationships.
Gabe Lupu indicated no relevant financial relationships.
Joyce Badal indicated no relevant financial relationships.
David Seligson indicated no relevant financial relationships.
Hanna Sanoff: Amgen – Grant/Research Support. AstraZeneca – Grant/Research Support. Biomed Valley Discoveries – Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Exelis – Grant/Research Support. F Hoffman La Roche – Grant/Research Support. Pfizer – Grant/Research Support. Rgenix – Grant/Research Support.
David Mauro indicated no relevant financial relationships.
David Gerber: Medtronic – Consultant.
Ted Yanagihara indicated no relevant financial relationships.
Alfred Barritt: Boehringer Ingelheim – Consultant. Merck (Any division) – Consultant. TARGET RWE – Consultant.
Andrew Moon: DCN Diagnostics – Grant/Research Support. Intercept – Advisory Committee/Board Member. TARGET RWE – Consultant.
Chidi Iloabachie, BS1, Yue Jiang, PhD2, Sydney Power, MD3, Arjun Juneja, BS4, Merete Lund, MD3, Gabe Lupu, MD3, Joyce Badal, MD4, David Seligson, MS5, Hanna Sanoff, MD3, David Mauro, MD3, David Gerber, MD4, Ted Yanagihara, MD3, Alfred S. Barritt, MD, MSCR6, Andrew Moon, MD, MPH3. P4625 - Associations Between Liver Disease Etiology and Post-Liver Directed Treatment Mortality in HCC, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

