Tuesday Poster Session
Category: Liver
P4798 - Atypical Presentation of Pylephlebitis: A Case of Proctitis and Portal Vein Thrombosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- IG
Isiah Gonzalez, MD (he/him/his)
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Isiah Gonzalez, MD, Ifeanyi Anyaoha, MD, Saltenat Moghaddam Adames, MD, Aya Hamadeh, MD, Danielle Morin, BS, Anita Kusnoor, MD
Baylor College of Medicine, Houston, TX
Introduction: Pylephlebitis, or infective suppurative thrombosis of the portal vein, is a rare condition associated with intra-abdominal infections and inflammation. Prompt treatment is crucial, as pylephlebitis carries a significant mortality risk. Pylephlebitis is typically associated with E. coli and Bacteroides and is most often associated with diverticulitis or acute appendicitis. We present a case of pylephlebitis in a patient with Bacteroides bacteriemia and severe proctitis.
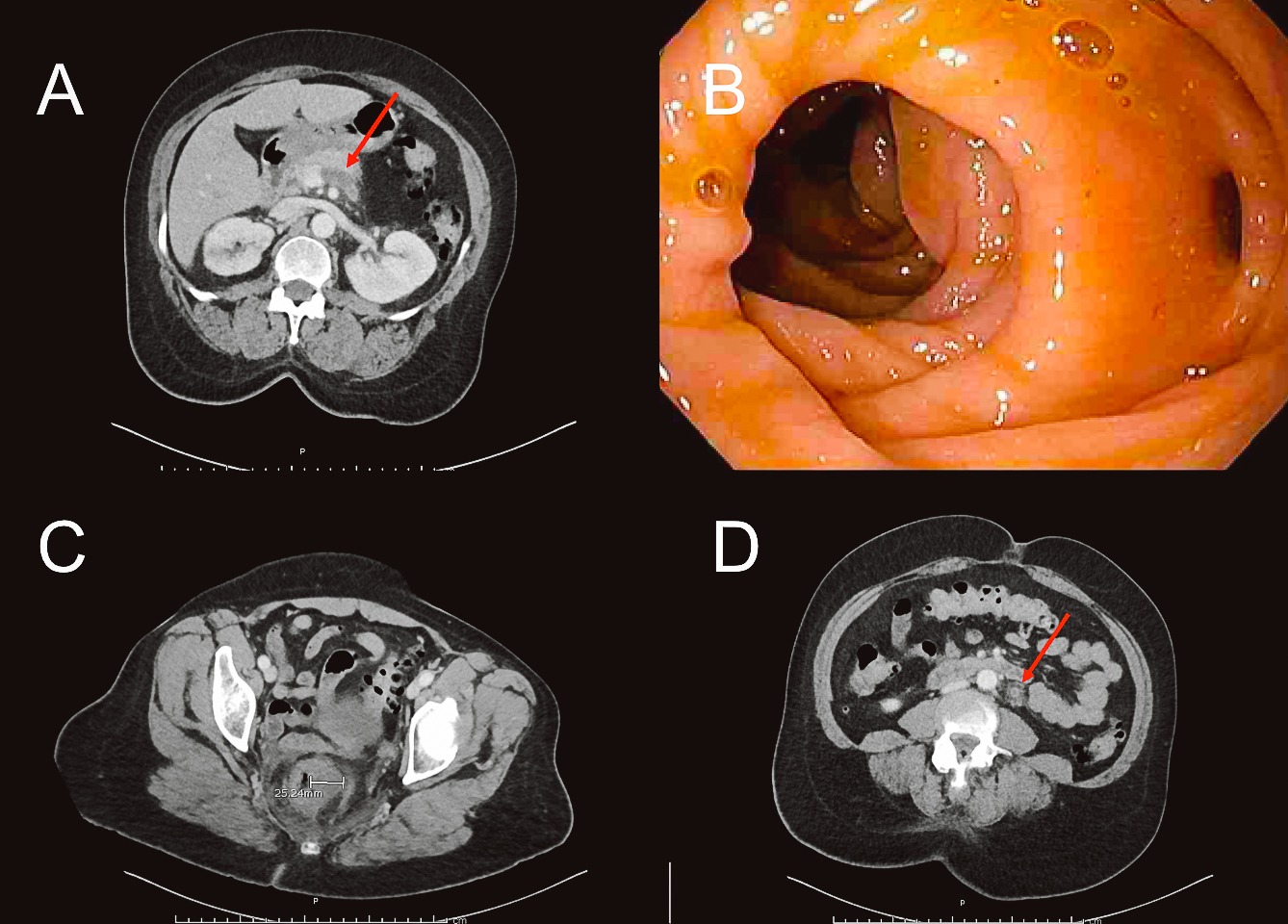
Case Description/Methods: A 60-year-old woman with a history of diverticulitis, schizophrenia, and cocaine-use disorder presented with diffuse abdominal pain and erratic behavior. She was unable to provide a history. Vitals were notable for tachycardia at 106 beats/min. Physical examination showed diffuse abdominal tenderness. Labs were notable for WBC 15.9 x 10^9/L and Cr 1.8 mg/dL. On day 2, the patient remained afebrile with persistent leukocytosis. A non-contrast head CT, TSH, RPR, and B12 levels were normal. A urine drug screen was positive for cocaine. Urine and blood cultures were obtained. On day 3, the patient's abdominal pain worsened. CT abdomen and pelvis revealed severe proctitis, an occlusive thrombus extending throughout the inferior mesenteric vein and superior rectal veins, and a non-occlusive thrombus in the distal splenic and superior mesenteric veins. Blood cultures grew Bacteroides fragilis, and ceftriaxone, metronidazole, and therapeutic enoxaparin were initiated. On day 5, antimicrobials were broadened to meropenem and micafungin. Ivermectin was added due to concern for strongyloidiasis. On day 8, flexible sigmoidoscopy revealed diverticula and internal hemorrhoids, but no proctitis. On day 9, repeat CT showed improvement in proctitis and stable pylephlebitis. The patient was discharged on day 11 with apixaban for 90 days, and six weeks of metronidazole.
Discussion: In the pre-antibiotic era, pylephlebitis was nearly universally fatal. It continues to pose a significant mortality risk of 10-14%. A triad of abdominal pain, fever, and leukocytosis is often observed, with our patient presenting with abdominal pain and leukocytosis. This case represents an atypical pylephlebitis presentation, characterized by the absence of diverticulitis, or appendicitis, and delayed onset of fever. Additionally, it demonstrates how cognitive biases such as premature closure may delay management and emphasizes the importance of prioritizing the chief complaint, especially with AMS, in guiding management.
Disclosures:
Isiah Gonzalez, MD, Ifeanyi Anyaoha, MD, Saltenat Moghaddam Adames, MD, Aya Hamadeh, MD, Danielle Morin, BS, Anita Kusnoor, MD. P4798 - Atypical Presentation of Pylephlebitis: A Case of Proctitis and Portal Vein Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Baylor College of Medicine, Houston, TX
Introduction: Pylephlebitis, or infective suppurative thrombosis of the portal vein, is a rare condition associated with intra-abdominal infections and inflammation. Prompt treatment is crucial, as pylephlebitis carries a significant mortality risk. Pylephlebitis is typically associated with E. coli and Bacteroides and is most often associated with diverticulitis or acute appendicitis. We present a case of pylephlebitis in a patient with Bacteroides bacteriemia and severe proctitis.
Case Description/Methods: A 60-year-old woman with a history of diverticulitis, schizophrenia, and cocaine-use disorder presented with diffuse abdominal pain and erratic behavior. She was unable to provide a history. Vitals were notable for tachycardia at 106 beats/min. Physical examination showed diffuse abdominal tenderness. Labs were notable for WBC 15.9 x 10^9/L and Cr 1.8 mg/dL. On day 2, the patient remained afebrile with persistent leukocytosis. A non-contrast head CT, TSH, RPR, and B12 levels were normal. A urine drug screen was positive for cocaine. Urine and blood cultures were obtained. On day 3, the patient's abdominal pain worsened. CT abdomen and pelvis revealed severe proctitis, an occlusive thrombus extending throughout the inferior mesenteric vein and superior rectal veins, and a non-occlusive thrombus in the distal splenic and superior mesenteric veins. Blood cultures grew Bacteroides fragilis, and ceftriaxone, metronidazole, and therapeutic enoxaparin were initiated. On day 5, antimicrobials were broadened to meropenem and micafungin. Ivermectin was added due to concern for strongyloidiasis. On day 8, flexible sigmoidoscopy revealed diverticula and internal hemorrhoids, but no proctitis. On day 9, repeat CT showed improvement in proctitis and stable pylephlebitis. The patient was discharged on day 11 with apixaban for 90 days, and six weeks of metronidazole.
Discussion: In the pre-antibiotic era, pylephlebitis was nearly universally fatal. It continues to pose a significant mortality risk of 10-14%. A triad of abdominal pain, fever, and leukocytosis is often observed, with our patient presenting with abdominal pain and leukocytosis. This case represents an atypical pylephlebitis presentation, characterized by the absence of diverticulitis, or appendicitis, and delayed onset of fever. Additionally, it demonstrates how cognitive biases such as premature closure may delay management and emphasizes the importance of prioritizing the chief complaint, especially with AMS, in guiding management.
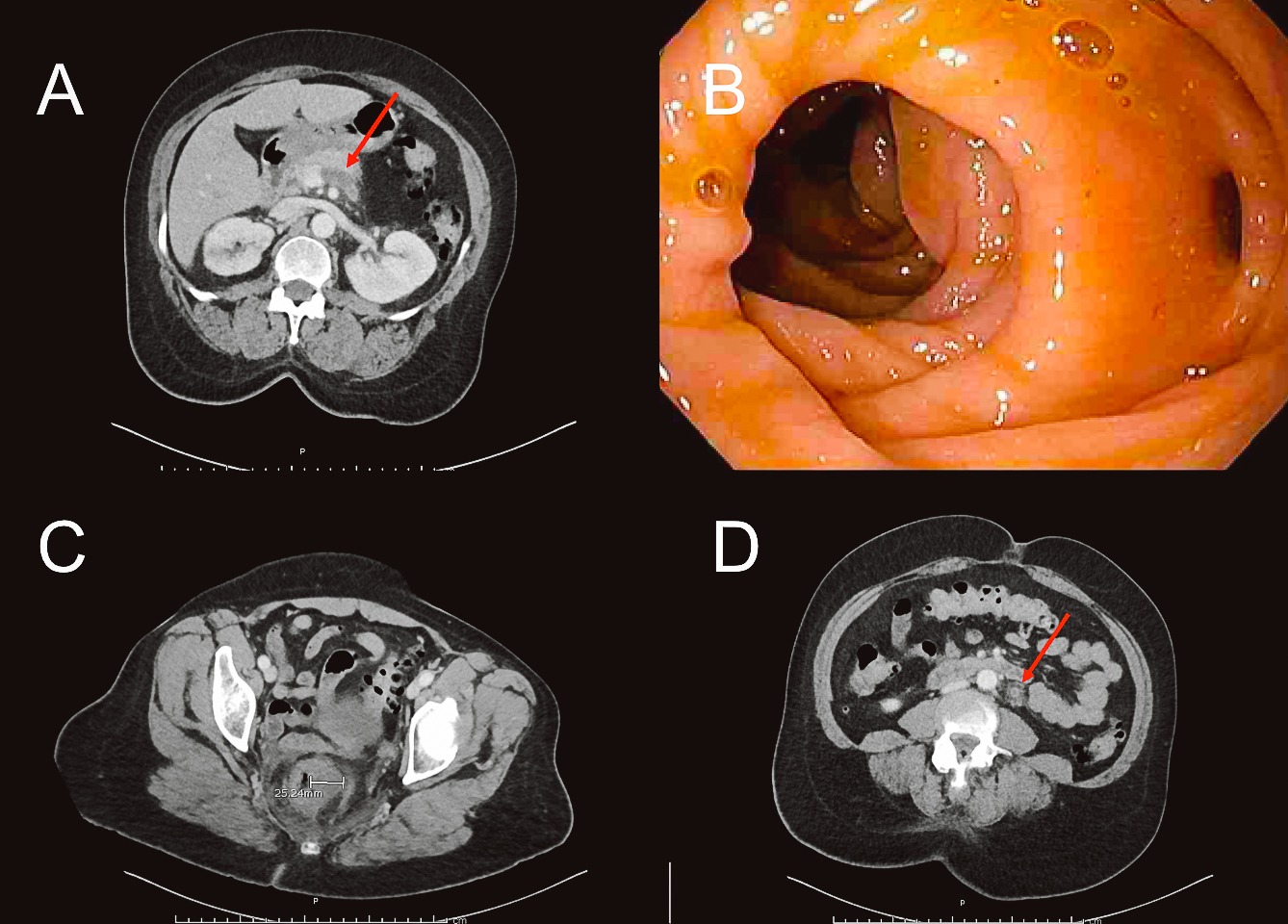
Figure: A: Non-occlusive thrombus at the confluence of the splenic and portal vein
B: Diverticula without diverticulitis
C: Rectal thickening
D: Fat surrounding the internal mesenteric vein, absent contrast
B: Diverticula without diverticulitis
C: Rectal thickening
D: Fat surrounding the internal mesenteric vein, absent contrast
Disclosures:
Isiah Gonzalez indicated no relevant financial relationships.
Ifeanyi Anyaoha indicated no relevant financial relationships.
Saltenat Moghaddam Adames indicated no relevant financial relationships.
Aya Hamadeh indicated no relevant financial relationships.
Danielle Morin indicated no relevant financial relationships.
Anita Kusnoor indicated no relevant financial relationships.
Isiah Gonzalez, MD, Ifeanyi Anyaoha, MD, Saltenat Moghaddam Adames, MD, Aya Hamadeh, MD, Danielle Morin, BS, Anita Kusnoor, MD. P4798 - Atypical Presentation of Pylephlebitis: A Case of Proctitis and Portal Vein Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
