Tuesday Poster Session
Category: Liver
P4800 - Unraveling the Connection: Autoimmune Hepatitis Coexisting With Psoriasis and Alcohol Use Disorder: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Nicole E. Villa, MD (she/her/hers)
NYC Health + Hospitals/Metropolitan
New York, NY
Presenting Author(s)
Nicole E. Villa, MD, Bede N. Nriagu, MD, MPH, Fnu Samaksh Sharma, MD, Oladimeji E. Oluaderounmu, MD, Noella Boma, MD
NYC Health + Hospitals/Metropolitan, New York, NY
Introduction: Autoimmune hepatitis (AIH) is characterized by chronic inflammation of the liver. It has varied clinical presentations, including acute liver failure. It is commonly associated with other autoimmune conditions, can occur at any age, and is more common among females. The exact pathogenesis is unknown, and it is a diagnosis of exclusion based on clinical, histologic, and laboratory findings. We report a case of a 41-year-old male presenting with painless jaundice.
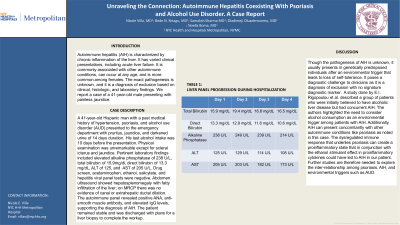
Case Description/Methods: A 41-year-old Hispanic man with a past medical history of hypertension, psoriasis, and alcohol use disorder (AUD) presented to the emergency department with pruritus, jaundice, and darkened urine of 14 days duration. His last alcohol intake was 10 days before the presentation. Physical examination was unremarkable except for scleral icterus and jaundice. Pertinent laboratory findings included elevated alkaline phosphatase of 238 U/L, total bilirubin of 15.9mg/dl, direct bilirubin of 13.3 mg/dL, ALT of 125, and AST of 205 U/L. Drug screen, acetaminophen, ethanol, salicylate, and hepatitis viral panel tests were negative. Abdomen ultrasound showed hepatosplenomegaly with fatty infiltration of the liver; on MRCP there was no evidence of canal or extrahepatic ductal dilation. The autoimmune panel revealed positive ANA, anti-smooth muscle antibody, and elevated IgG levels, supporting the diagnosis of AIH. The patient remained stable and was discharged with plans for a liver biopsy to complete the workup.
Discussion: Though the pathogenesis of AIH is unknown, it usually presents in genetically predisposed individuals after an environmental trigger that leads to loss of self-tolerance. It poses a diagnostic challenge to clinicians as it is a diagnosis of exclusion with no signature diagnostic marker. A study done by E.I. Rigopoulou et al. described a group of patients who were initially believed to have alcoholic liver disease but had concurrent AIH. The authors highlighted the need to consider alcohol consumption as an environmental trigger among patients with AIH. Additionally, AIH can present concomitantly with other autoimmune conditions like psoriasis as noted in this case. The dysregulated immune response that underlies psoriasis can create a proinflammatory state that in conjunction with the ethanol stimulant effect in proinflammatory cytokines could have led to AIH in our patient. Further studies are therefore needed to explore the inter-relationship among psoriasis, AIH, and environmental triggers such as AUD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nicole E. Villa, MD, Bede N. Nriagu, MD, MPH, Fnu Samaksh Sharma, MD, Oladimeji E. Oluaderounmu, MD, Noella Boma, MD. P4800 - Unraveling the Connection: Autoimmune Hepatitis Coexisting With Psoriasis and Alcohol Use Disorder: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
NYC Health + Hospitals/Metropolitan, New York, NY
Introduction: Autoimmune hepatitis (AIH) is characterized by chronic inflammation of the liver. It has varied clinical presentations, including acute liver failure. It is commonly associated with other autoimmune conditions, can occur at any age, and is more common among females. The exact pathogenesis is unknown, and it is a diagnosis of exclusion based on clinical, histologic, and laboratory findings. We report a case of a 41-year-old male presenting with painless jaundice.
Case Description/Methods: A 41-year-old Hispanic man with a past medical history of hypertension, psoriasis, and alcohol use disorder (AUD) presented to the emergency department with pruritus, jaundice, and darkened urine of 14 days duration. His last alcohol intake was 10 days before the presentation. Physical examination was unremarkable except for scleral icterus and jaundice. Pertinent laboratory findings included elevated alkaline phosphatase of 238 U/L, total bilirubin of 15.9mg/dl, direct bilirubin of 13.3 mg/dL, ALT of 125, and AST of 205 U/L. Drug screen, acetaminophen, ethanol, salicylate, and hepatitis viral panel tests were negative. Abdomen ultrasound showed hepatosplenomegaly with fatty infiltration of the liver; on MRCP there was no evidence of canal or extrahepatic ductal dilation. The autoimmune panel revealed positive ANA, anti-smooth muscle antibody, and elevated IgG levels, supporting the diagnosis of AIH. The patient remained stable and was discharged with plans for a liver biopsy to complete the workup.
Discussion: Though the pathogenesis of AIH is unknown, it usually presents in genetically predisposed individuals after an environmental trigger that leads to loss of self-tolerance. It poses a diagnostic challenge to clinicians as it is a diagnosis of exclusion with no signature diagnostic marker. A study done by E.I. Rigopoulou et al. described a group of patients who were initially believed to have alcoholic liver disease but had concurrent AIH. The authors highlighted the need to consider alcohol consumption as an environmental trigger among patients with AIH. Additionally, AIH can present concomitantly with other autoimmune conditions like psoriasis as noted in this case. The dysregulated immune response that underlies psoriasis can create a proinflammatory state that in conjunction with the ethanol stimulant effect in proinflammatory cytokines could have led to AIH in our patient. Further studies are therefore needed to explore the inter-relationship among psoriasis, AIH, and environmental triggers such as AUD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nicole Villa indicated no relevant financial relationships.
Bede Nriagu indicated no relevant financial relationships.
Fnu Samaksh Sharma indicated no relevant financial relationships.
Oladimeji Oluaderounmu indicated no relevant financial relationships.
Noella Boma indicated no relevant financial relationships.
Nicole E. Villa, MD, Bede N. Nriagu, MD, MPH, Fnu Samaksh Sharma, MD, Oladimeji E. Oluaderounmu, MD, Noella Boma, MD. P4800 - Unraveling the Connection: Autoimmune Hepatitis Coexisting With Psoriasis and Alcohol Use Disorder: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
