Tuesday Poster Session
Category: Liver
P4762 - Unique Case of Vanishing Bile Duct Syndrome Exacerbated by Noncompliance
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Michael Farber, BS (he/him/his)
NYIT College of Osteopathic Medicine
Glen Head, NY
Presenting Author(s)
Michael Farber, BS1, Garvita Sharma, BA2, Nicholas Condiles, MD3
1NYIT College of Osteopathic Medicine, Glen Head, NY; 2Arkansas College of Osteopathic Medicine, Albertson, NY; 3North Shore University Hospital - Northwell Health, Manhasset, NY
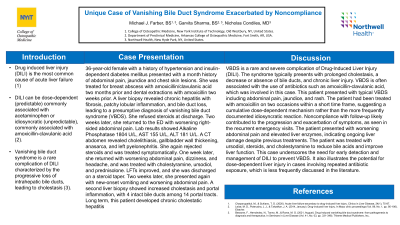
Introduction: Drug induced liver injury (DILI) is the most common cause of liver injury. It can be dose-dependent, commonly associated with acetaminophen1 or idiosyncratic, associated with amoxicillin-clavulanic acid2. In a small subset of patients, DILI may lead to vanishing bile duct syndrome (VBDS)2, a prolonged cholestatic injury marked by loss of intrahepatic bile ducts.
Case Description/Methods: This is the case of a 36-year-old female with a history of hypertension and type 1 DM. She reported a one-month history of jaundice, chest skin lesions and a one-year history of 100 lb weight loss. She was treated for an abscess with amoxicillin/clavulanic acid two months earlier and for a dental procedure with amoxicillin two weeks earlier. A liver biopsy revealed chronic hepatitis, increased fibrosis, patchy lobular inflammation, hepatic lobules and bile duct loss, with a presumptive diagnosis of VBDS.
Due to noncompliance, the patient presented to the ED two weeks later with worsening right-sided abdominal pain. Lab results showed: ALP 1804, AST 155, ALT 181 and positive celiac IgA. A CT A/P revealed cholelithiasis, gallbladder mural thickening, anasarca and left pyelonephritis. She was treated symptomatically and discharged after improvement in liver function tests (LFTs) with presumed celiac disease and DILI diagnoses
One week later, the patient returned to the ED with worsening abdominal pain, headache and dizziness. She was treated with cholestyramine, ursodiol, simethicone, maalox, and prednisolone. LFTs improved and she was discharged with outpatient follow up.
Two weeks later, the patient returned to the ED due to non-bloody, non-bilious vomiting and worsening epigastric and upper quadrant abdominal pain. At discharge, AST was 83 and ALT 108. A CTAP was consistent with prior findings, and repeated liver biopsy revealed an increase in cholestasis with intraductal bile, bile lakes and increased portal inflammation. She was treated with the same regimen as the last hospital stay.
Discussion: VBDS is a rare complication of DILI. Presentation with immunoallergic symptoms such as jaundice, rash, and fatigue are typical. Elevated labs such as ALP, lipid profiles and total bilirubin are often consistent with a diagnosis of VBDS3. The patient was prescribed both amoxicillin and amoxicillin-clavulanic acid within a 3 month period which points to dose-dependent cause, which differs from the more documented idiosyncratic cause. This case was unique because of the exacerbated nature of disease due to noncompliance.
Disclosures:
Michael Farber, BS1, Garvita Sharma, BA2, Nicholas Condiles, MD3. P4762 - Unique Case of Vanishing Bile Duct Syndrome Exacerbated by Noncompliance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYIT College of Osteopathic Medicine, Glen Head, NY; 2Arkansas College of Osteopathic Medicine, Albertson, NY; 3North Shore University Hospital - Northwell Health, Manhasset, NY
Introduction: Drug induced liver injury (DILI) is the most common cause of liver injury. It can be dose-dependent, commonly associated with acetaminophen1 or idiosyncratic, associated with amoxicillin-clavulanic acid2. In a small subset of patients, DILI may lead to vanishing bile duct syndrome (VBDS)2, a prolonged cholestatic injury marked by loss of intrahepatic bile ducts.
Case Description/Methods: This is the case of a 36-year-old female with a history of hypertension and type 1 DM. She reported a one-month history of jaundice, chest skin lesions and a one-year history of 100 lb weight loss. She was treated for an abscess with amoxicillin/clavulanic acid two months earlier and for a dental procedure with amoxicillin two weeks earlier. A liver biopsy revealed chronic hepatitis, increased fibrosis, patchy lobular inflammation, hepatic lobules and bile duct loss, with a presumptive diagnosis of VBDS.
Due to noncompliance, the patient presented to the ED two weeks later with worsening right-sided abdominal pain. Lab results showed: ALP 1804, AST 155, ALT 181 and positive celiac IgA. A CT A/P revealed cholelithiasis, gallbladder mural thickening, anasarca and left pyelonephritis. She was treated symptomatically and discharged after improvement in liver function tests (LFTs) with presumed celiac disease and DILI diagnoses
One week later, the patient returned to the ED with worsening abdominal pain, headache and dizziness. She was treated with cholestyramine, ursodiol, simethicone, maalox, and prednisolone. LFTs improved and she was discharged with outpatient follow up.
Two weeks later, the patient returned to the ED due to non-bloody, non-bilious vomiting and worsening epigastric and upper quadrant abdominal pain. At discharge, AST was 83 and ALT 108. A CTAP was consistent with prior findings, and repeated liver biopsy revealed an increase in cholestasis with intraductal bile, bile lakes and increased portal inflammation. She was treated with the same regimen as the last hospital stay.
Discussion: VBDS is a rare complication of DILI. Presentation with immunoallergic symptoms such as jaundice, rash, and fatigue are typical. Elevated labs such as ALP, lipid profiles and total bilirubin are often consistent with a diagnosis of VBDS3. The patient was prescribed both amoxicillin and amoxicillin-clavulanic acid within a 3 month period which points to dose-dependent cause, which differs from the more documented idiosyncratic cause. This case was unique because of the exacerbated nature of disease due to noncompliance.
Disclosures:
Michael Farber indicated no relevant financial relationships.
Garvita Sharma indicated no relevant financial relationships.
Nicholas Condiles indicated no relevant financial relationships.
Michael Farber, BS1, Garvita Sharma, BA2, Nicholas Condiles, MD3. P4762 - Unique Case of Vanishing Bile Duct Syndrome Exacerbated by Noncompliance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
