Sunday Poster Session
Category: Pediatrics
P1481 - A Rare Case of Overlapping Eosinophilic Granulomatosis With Polyangiitis and Crohn's Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- BM
Brooke McVaney, DO (she/her/hers)
LSU Health New Orleans School of Medicine
New Orleans, LA
Presenting Author(s)
Brooke McVaney, DO1, Amber Gafur, MD1, Salim C.. Lutfallah, BS2, Holly Breeden, MD1, Elizabeth McDonough, MD1, Colleen Leblanc, MD1
1LSU Health New Orleans School of Medicine, New Orleans, LA; 2LSU Health New Orleans School of Medicine, Metairie, LA
Introduction: Eosinophilic granulomatosis with polyangiitis (EGPA) is a vasculitis of small and medium sized arteries. EGPA is rare in the pediatric population with only 33 published case reports. It is a multisystem disease that can affect any organ system. Crohn’s Disease is a type of inflammatory bowel disease (IBD) that can affect any segment of the gastrointestinal (GI) tract and is also associated with a wide variety of extraintestinal manifestations. We present a case of diagnosis of IBD following presentation of EGPA.
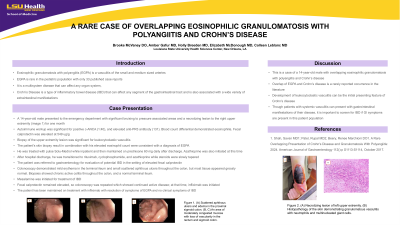
Case Description/Methods: A 14-year-old male presented with significant bruising to pressure associated areas and a necrotizing lesion to the right upper extremity for one month. Autoimmune workup was significant for positive c-ANCA (1:40), and elevated anti-PR3 antibody (131). Infectious workup was negative. Blood count differential demonstrated eosinophilia with an absolute eosinophil count of 3.12 10ˆ3/uL. Fecal calprotectin was elevated at 549 ug/g.
Biopsy of the upper extremity lesion was significant for small and medium vessel vasculitis. The patient's skin biopsy result in combination with his elevated eosinophil count were consistent with a diagnosis of EGPA. He was treated with Solu-Medrol while inpatient and was discharged on prednisone and azathioprine. His eosinophil count normalized during steroid treatment. Following hospital discharge, his treatment for EGPA was then transitioned to rituximab, cyclophosphamide, and azathioprine while steroids were slowly tapered.
The patient was referred to gastroenterology for evaluation of potential IBD in the setting of elevated fecal calprotectin. Colonoscopy demonstrated congested and erythematous mucosa of the entire examined colon, and erythematous and congested mucosa in the terminal ileum. Histology showed chronic active colitis of the entire biopsied colon. Findings were consistent with Crohn’s Disease. Mesalamine was initiated for treatment of IBD.
The patient has been maintained on treatment with rituximab every six months and mesalamine 3.6 g daily with resolution of symptoms of EGPA and no symptoms of IBD.
Discussion: This is a case of a 14-year-old male with overlapping eosinophilic granulomatosis with polyangiitis and Crohn’s disease. Overlap of EGPA and Crohn’s disease is a rarely reported occurrence in the literature. Though patients with systemic vasculitis can present with gastrointestinal manifestations of their disease, it is important to screen for IBD if GI symptoms are present in this patient population.

Disclosures:
Brooke McVaney, DO1, Amber Gafur, MD1, Salim C.. Lutfallah, BS2, Holly Breeden, MD1, Elizabeth McDonough, MD1, Colleen Leblanc, MD1. P1481 - A Rare Case of Overlapping Eosinophilic Granulomatosis With Polyangiitis and Crohn's Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1LSU Health New Orleans School of Medicine, New Orleans, LA; 2LSU Health New Orleans School of Medicine, Metairie, LA
Introduction: Eosinophilic granulomatosis with polyangiitis (EGPA) is a vasculitis of small and medium sized arteries. EGPA is rare in the pediatric population with only 33 published case reports. It is a multisystem disease that can affect any organ system. Crohn’s Disease is a type of inflammatory bowel disease (IBD) that can affect any segment of the gastrointestinal (GI) tract and is also associated with a wide variety of extraintestinal manifestations. We present a case of diagnosis of IBD following presentation of EGPA.
Case Description/Methods: A 14-year-old male presented with significant bruising to pressure associated areas and a necrotizing lesion to the right upper extremity for one month. Autoimmune workup was significant for positive c-ANCA (1:40), and elevated anti-PR3 antibody (131). Infectious workup was negative. Blood count differential demonstrated eosinophilia with an absolute eosinophil count of 3.12 10ˆ3/uL. Fecal calprotectin was elevated at 549 ug/g.
Biopsy of the upper extremity lesion was significant for small and medium vessel vasculitis. The patient's skin biopsy result in combination with his elevated eosinophil count were consistent with a diagnosis of EGPA. He was treated with Solu-Medrol while inpatient and was discharged on prednisone and azathioprine. His eosinophil count normalized during steroid treatment. Following hospital discharge, his treatment for EGPA was then transitioned to rituximab, cyclophosphamide, and azathioprine while steroids were slowly tapered.
The patient was referred to gastroenterology for evaluation of potential IBD in the setting of elevated fecal calprotectin. Colonoscopy demonstrated congested and erythematous mucosa of the entire examined colon, and erythematous and congested mucosa in the terminal ileum. Histology showed chronic active colitis of the entire biopsied colon. Findings were consistent with Crohn’s Disease. Mesalamine was initiated for treatment of IBD.
The patient has been maintained on treatment with rituximab every six months and mesalamine 3.6 g daily with resolution of symptoms of EGPA and no symptoms of IBD.
Discussion: This is a case of a 14-year-old male with overlapping eosinophilic granulomatosis with polyangiitis and Crohn’s disease. Overlap of EGPA and Crohn’s disease is a rarely reported occurrence in the literature. Though patients with systemic vasculitis can present with gastrointestinal manifestations of their disease, it is important to screen for IBD if GI symptoms are present in this patient population.

Figure: Right upper extremity skin lesion
Disclosures:
Brooke McVaney indicated no relevant financial relationships.
Amber Gafur indicated no relevant financial relationships.
Salim Lutfallah indicated no relevant financial relationships.
Holly Breeden indicated no relevant financial relationships.
Elizabeth McDonough indicated no relevant financial relationships.
Colleen Leblanc indicated no relevant financial relationships.
Brooke McVaney, DO1, Amber Gafur, MD1, Salim C.. Lutfallah, BS2, Holly Breeden, MD1, Elizabeth McDonough, MD1, Colleen Leblanc, MD1. P1481 - A Rare Case of Overlapping Eosinophilic Granulomatosis With Polyangiitis and Crohn's Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
