Tuesday Poster Session
Category: General Endoscopy
P4128 - Gastric Ulcer Disease Presenting as Acute Pancreatitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Alana B. Barofsky, MD
Saint Peter's University Hospital
New Brunswick, NJ
Presenting Author(s)
Boris Livitz, MD1, Alana B. Barofsky, MD2, Nazir Ahmed, MD3, Shawn Philip, DO3, Davood K Hosseini, MD3, Uri Hochfeld, MD3, Jonathan Weinberger, MD3
1Stony Brook Southampton Hospital, Patchogue, NY; 2Saint Peter's University Hospital, New Brunswick, NJ; 3Hackensack University Medical Center, Hackensack, NJ
Introduction: Acute pancreatitis is diagnosed based on the Atlanta criteria: i) typical pain, ii) serum lipase/amylase levels greater than three times, and/or iii) characteristic imaging findings. In addition to pancreatitis, lipase levels are also elevated in small-bowel, hepatobiliary and renal pathology in addition to other rare causes. We describe a case of a patient with elevated lipase with normal pancreas.
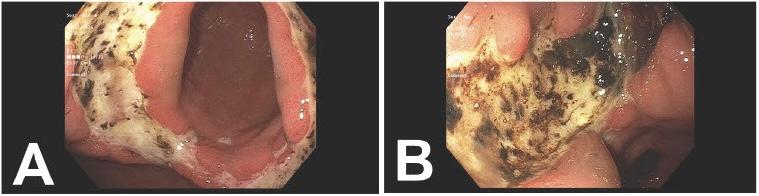
Case Description/Methods: A 34-year-old male without any medical history presented with sharp epigastric pain aggravated by food for two days. This was associated with episodes of bilious emesis. He denied alcohol abuse or use of any new medicines. Patient had normal vitals and on exam he had epigastric and periumbilical tenderness. Laboratory studies showed leukocytosis of 18.1x109/L, hemoglobin 17 g/dL, hematocrit 51% and normal platelets. His liver chemistry was noted to be within normal range including AST 39 U/L, ALT 43 U/L, ALP 88 U/L and bilirubin 0.5 mg/dL. His lipase was elevated at 615 U/LA. Ultrasound revealed cholelithiasis without cholecystitis and normal bile ducts. The patient was managed with IV fluids for suspected acute gallstone pancreatitis and was scheduled to undergo cholecystectomy after surgical evaluation. A follow-up CT scan showed normal pancreas but did note diffuse gastric antrum mucosal edema consistent with gastritis. Gastroenterology was consulted and upon further history, he reported daily ibuprofen use for months. Subsequent endoscopic evaluation revealed multiple gastric ulcers in the gastric antrum with the largest being nearly circumferential involving the incisura and extending into the greater curvature. Biopsy revealed acute gastritis with negative H. Pylori. The patient was diagnosed with NSAID induced gastric ulcers and discharged on twice-daily pantoprazole therapy with advice to follow up for repeat endoscopy to assess healing.
Discussion: In our case, the patient was diagnosed with acute pancreatitis based on Atlanta criteria and planned for further surgical intervention due to his noted gallstones. Further diagnostic workup, which in this specific scenario was not strongly indicated, revealed gastric ulcers without any pancreatic disease or duodenal ulcers. Though lipase levels greater than three times the upper limit of normal are highly sensitive and specific for pancreatitis, it is important to obtain a thorough history to help guide diagnosis and provide appropriate management.
Disclosures:
Boris Livitz, MD1, Alana B. Barofsky, MD2, Nazir Ahmed, MD3, Shawn Philip, DO3, Davood K Hosseini, MD3, Uri Hochfeld, MD3, Jonathan Weinberger, MD3. P4128 - Gastric Ulcer Disease Presenting as Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Stony Brook Southampton Hospital, Patchogue, NY; 2Saint Peter's University Hospital, New Brunswick, NJ; 3Hackensack University Medical Center, Hackensack, NJ
Introduction: Acute pancreatitis is diagnosed based on the Atlanta criteria: i) typical pain, ii) serum lipase/amylase levels greater than three times, and/or iii) characteristic imaging findings. In addition to pancreatitis, lipase levels are also elevated in small-bowel, hepatobiliary and renal pathology in addition to other rare causes. We describe a case of a patient with elevated lipase with normal pancreas.
Case Description/Methods: A 34-year-old male without any medical history presented with sharp epigastric pain aggravated by food for two days. This was associated with episodes of bilious emesis. He denied alcohol abuse or use of any new medicines. Patient had normal vitals and on exam he had epigastric and periumbilical tenderness. Laboratory studies showed leukocytosis of 18.1x109/L, hemoglobin 17 g/dL, hematocrit 51% and normal platelets. His liver chemistry was noted to be within normal range including AST 39 U/L, ALT 43 U/L, ALP 88 U/L and bilirubin 0.5 mg/dL. His lipase was elevated at 615 U/LA. Ultrasound revealed cholelithiasis without cholecystitis and normal bile ducts. The patient was managed with IV fluids for suspected acute gallstone pancreatitis and was scheduled to undergo cholecystectomy after surgical evaluation. A follow-up CT scan showed normal pancreas but did note diffuse gastric antrum mucosal edema consistent with gastritis. Gastroenterology was consulted and upon further history, he reported daily ibuprofen use for months. Subsequent endoscopic evaluation revealed multiple gastric ulcers in the gastric antrum with the largest being nearly circumferential involving the incisura and extending into the greater curvature. Biopsy revealed acute gastritis with negative H. Pylori. The patient was diagnosed with NSAID induced gastric ulcers and discharged on twice-daily pantoprazole therapy with advice to follow up for repeat endoscopy to assess healing.
Discussion: In our case, the patient was diagnosed with acute pancreatitis based on Atlanta criteria and planned for further surgical intervention due to his noted gallstones. Further diagnostic workup, which in this specific scenario was not strongly indicated, revealed gastric ulcers without any pancreatic disease or duodenal ulcers. Though lipase levels greater than three times the upper limit of normal are highly sensitive and specific for pancreatitis, it is important to obtain a thorough history to help guide diagnosis and provide appropriate management.
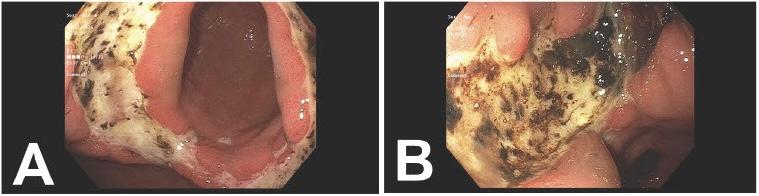
Figure: A. Gastric antral ulcer B. Incisura
Disclosures:
Boris Livitz indicated no relevant financial relationships.
Alana Barofsky indicated no relevant financial relationships.
Nazir Ahmed indicated no relevant financial relationships.
Shawn Philip indicated no relevant financial relationships.
Davood K Hosseini indicated no relevant financial relationships.
Uri Hochfeld indicated no relevant financial relationships.
Jonathan Weinberger indicated no relevant financial relationships.
Boris Livitz, MD1, Alana B. Barofsky, MD2, Nazir Ahmed, MD3, Shawn Philip, DO3, Davood K Hosseini, MD3, Uri Hochfeld, MD3, Jonathan Weinberger, MD3. P4128 - Gastric Ulcer Disease Presenting as Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
