Tuesday Poster Session
Category: GI Bleeding
P4207 - From Lifesaving to Life Threatening: Intravascular Embolization Coil Migration Resulting in Perforated Gastric Ulcer and Hemorrhagic Shock
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sarah Herrera Mercedes, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Sarah Herrera Mercedes, MD, Sierra Anderson, MD, Zoë Post, MD, Atsushi Sakuraba, MD
Rush University Medical Center, Chicago, IL
Introduction: Endoscopic hemostasis is the standard treatment for upper gastrointestinal bleeding (UGIB). When unable to achieve hemostasis endoscopically, trans-arterial embolization is an alternative. Effective trans-arterial coil embolization can be complicated by non-target vessel occlusion, vessel dissection, ischemia, perforation, and coil migration. In most cases, coil migration involves spontaneous healing without serious complications. Here we describe coil migration complicated by hemorrhagic shock and gastric perforation, bringing awareness to this life-threatening complication.
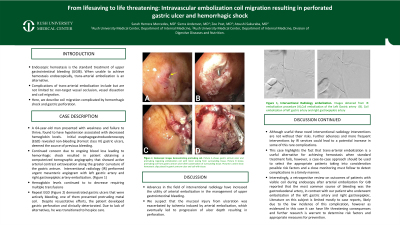
Case Description/Methods: A 64-year-old man presented with weakness and failure to thrive, found to have hypotension associated with decreased hemoglobin levels, requiring ICU admission. Initial esophagogastroduodenoscopy (EGD) revealed non-bleeding (Forrest class III) gastric ulcers, deemed the source of previous bleeding. However, due to continued concern for ongoing blood loss leading to hemorrhagic shock, a computerized tomographic angiography was obtained, showing active arterial contrast extravasation along the greater curvature of the gastric antrum. Interventional radiology performed an urgent mesenteric angiogram with left gastric artery and right gastroepiploic artery embolization, but hemoglobin levels continued to decrease, requiring multiple transfusions. Repeat EGD demonstrated gastric ulcers that were now bleeding and one with a protruding metal coil. Hemostasis was attempted using bipolar probe and subsequently solution of epinephrine, followed by hemostatic spray. There was no bleeding at the end of the procedure, and three hemostatic clips were placed to prevent bleeding post-intervention. Despite resuscitative efforts, the patient developed gastric perforation and clinically deteriorated. Due to a lack of alternative options, he transitioned to hospice care and eventually passed away.
Discussion: This case demonstrates that a life-saving intervention can lead to a life-threatening complication. Advances in the field of interventional radiology have increased the utility of arterial embolization in the management of UGIB. While mostly successful, these procedures are not without risk. We suspect that the mucosal injury from ulceration was exacerbated by ischemia induced by arterial embolization, leading to the progression of ulcer depth and resulting in perforation. This suggests that the presence of gastric ulcers with associated mucosal injury significantly increases complication risk.

Disclosures:
Sarah Herrera Mercedes, MD, Sierra Anderson, MD, Zoë Post, MD, Atsushi Sakuraba, MD. P4207 - From Lifesaving to Life Threatening: Intravascular Embolization Coil Migration Resulting in Perforated Gastric Ulcer and Hemorrhagic Shock, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Endoscopic hemostasis is the standard treatment for upper gastrointestinal bleeding (UGIB). When unable to achieve hemostasis endoscopically, trans-arterial embolization is an alternative. Effective trans-arterial coil embolization can be complicated by non-target vessel occlusion, vessel dissection, ischemia, perforation, and coil migration. In most cases, coil migration involves spontaneous healing without serious complications. Here we describe coil migration complicated by hemorrhagic shock and gastric perforation, bringing awareness to this life-threatening complication.
Case Description/Methods: A 64-year-old man presented with weakness and failure to thrive, found to have hypotension associated with decreased hemoglobin levels, requiring ICU admission. Initial esophagogastroduodenoscopy (EGD) revealed non-bleeding (Forrest class III) gastric ulcers, deemed the source of previous bleeding. However, due to continued concern for ongoing blood loss leading to hemorrhagic shock, a computerized tomographic angiography was obtained, showing active arterial contrast extravasation along the greater curvature of the gastric antrum. Interventional radiology performed an urgent mesenteric angiogram with left gastric artery and right gastroepiploic artery embolization, but hemoglobin levels continued to decrease, requiring multiple transfusions. Repeat EGD demonstrated gastric ulcers that were now bleeding and one with a protruding metal coil. Hemostasis was attempted using bipolar probe and subsequently solution of epinephrine, followed by hemostatic spray. There was no bleeding at the end of the procedure, and three hemostatic clips were placed to prevent bleeding post-intervention. Despite resuscitative efforts, the patient developed gastric perforation and clinically deteriorated. Due to a lack of alternative options, he transitioned to hospice care and eventually passed away.
Discussion: This case demonstrates that a life-saving intervention can lead to a life-threatening complication. Advances in the field of interventional radiology have increased the utility of arterial embolization in the management of UGIB. While mostly successful, these procedures are not without risk. We suspect that the mucosal injury from ulceration was exacerbated by ischemia induced by arterial embolization, leading to the progression of ulcer depth and resulting in perforation. This suggests that the presence of gastric ulcers with associated mucosal injury significantly increases complication risk.

Figure: Figure 1a: Initial non-bleeding gastric ulcer on the greater curvature of the gastric antrum found in first EGD. Figure 1b: Visible protruding coil from bleeding gastric ulcer found during final EGD in gastric antrum. Figures c & d: hemostatic clips to prevent post-intervention bleeding.
Disclosures:
Sarah Herrera Mercedes indicated no relevant financial relationships.
Sierra Anderson indicated no relevant financial relationships.
Zoë Post indicated no relevant financial relationships.
Atsushi Sakuraba indicated no relevant financial relationships.
Sarah Herrera Mercedes, MD, Sierra Anderson, MD, Zoë Post, MD, Atsushi Sakuraba, MD. P4207 - From Lifesaving to Life Threatening: Intravascular Embolization Coil Migration Resulting in Perforated Gastric Ulcer and Hemorrhagic Shock, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
