Sunday Poster Session
Category: Liver
P1197 - Impact of COVID-19 on Hospitalized Patients With and Without Liver Cirrhosis: Analysis of National Inpatient Sample 2020-2021
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- HU
Hameed Ullah, MD
Saint Luke's Hospital
St. Louis, MO
Presenting Author(s)
Hameed Ullah, MD1, Mohamad Sharbatji, MD2, Muhammad Jahanzaib Khan, MD3, Hasan Raza, MD4, Saeed Ali, MD5
1Saint Luke's Hospital, St. Louis, MO; 2AdventHealth Medical Group, AdventHealth, Orlando, FL; 3Mather Hospital, Northwell Health, New York, NY; 4University of Chicago Medical Center, Chicago, IL; 5AdventHealth, Orlando, FL
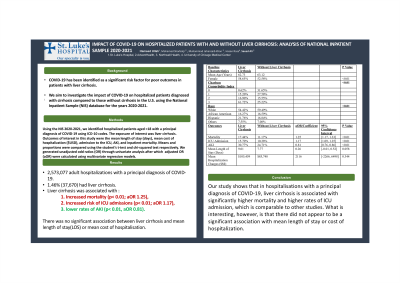
Introduction: Coronavirus disease 2019 (COVID-19) has been identified as a significant risk factor for poor outcomes in patients with liver cirrhosis. What makes this difficult to interpret is that there is a spectrum of severity with regards to patients with cirrhosis in terms of sequelae from portal hypertension and other comorbidities. We aim to investigate the impact of COVID-19 on hospitalized patients diagnosed with cirrhosis compared to those without cirrhosis in the U.S. using the National Inpatient Sample (NIS) database for the years 2020-2021.
Methods: Using the NIS 2020-2021, we identified hospitalized patients aged >18 with a principal diagnosis of COVID-19 using ICD-10 codes. The exposure of interest was liver cirrhosis. Outcomes of interest in this study were the mean length of stay (days), mean cost of hospitalization ($USD), admission to Iintensive Ccare Uunit (ICU), presence of Aacute Kkidney Iinjury, and inpatient mortality. Means and proportions were compared using the student’s t-test and chi-squared test respectively. We generated unadjusted odd ratios (OR) through univariate analysis after which an adjusted OR (aOR) were calculated using multivariate regression models.
Results: Of the 2,573,077 adult hospitalizations with a principal diagnosis of COVID-19, 1.46% (37,670) had been diagnosed with liver cirrhosis. Of these patients, 58.65% were female (p< 0.01), 54.42% were White, 16.27% were African American, and 21.76% were Hispanic (Table 1). Compared to patients without liver cirrhosis, liver cirrhosis was associated with significantly increased mortality (p< 0.01; aOR 1.25), increased risk of ICU admissions (p< 0.01; aOR 1.17), and significantly lower rates of AKI(p< 0.01, aOR 0.81). There was no significant association between liver cirrhosis and mean length of stay(LOS) or mean cost of hospitalisation.
Discussion: Our study shows that in hospitalisations with a principal diagnosis of COVID-19, liver cirrhosis is associated with significantly higher mortality and higher rates of ICU admission, which is comparable to other studies. What is interesting, however, is that there did not appear to be a significant association with mean length of stay or cost of hospitalization. With liver cirrhosis being a major risk factor for poor outcomes in the hospital setting, these findings warrant further investigation to identify how there is no significant difference between mean cost of hospitalization and mean LOS despite higher level of acuity and complexity of care in these patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hameed Ullah, MD1, Mohamad Sharbatji, MD2, Muhammad Jahanzaib Khan, MD3, Hasan Raza, MD4, Saeed Ali, MD5. P1197 - Impact of COVID-19 on Hospitalized Patients With and Without Liver Cirrhosis: Analysis of National Inpatient Sample 2020-2021, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Luke's Hospital, St. Louis, MO; 2AdventHealth Medical Group, AdventHealth, Orlando, FL; 3Mather Hospital, Northwell Health, New York, NY; 4University of Chicago Medical Center, Chicago, IL; 5AdventHealth, Orlando, FL
Introduction: Coronavirus disease 2019 (COVID-19) has been identified as a significant risk factor for poor outcomes in patients with liver cirrhosis. What makes this difficult to interpret is that there is a spectrum of severity with regards to patients with cirrhosis in terms of sequelae from portal hypertension and other comorbidities. We aim to investigate the impact of COVID-19 on hospitalized patients diagnosed with cirrhosis compared to those without cirrhosis in the U.S. using the National Inpatient Sample (NIS) database for the years 2020-2021.
Methods: Using the NIS 2020-2021, we identified hospitalized patients aged >18 with a principal diagnosis of COVID-19 using ICD-10 codes. The exposure of interest was liver cirrhosis. Outcomes of interest in this study were the mean length of stay (days), mean cost of hospitalization ($USD), admission to Iintensive Ccare Uunit (ICU), presence of Aacute Kkidney Iinjury, and inpatient mortality. Means and proportions were compared using the student’s t-test and chi-squared test respectively. We generated unadjusted odd ratios (OR) through univariate analysis after which an adjusted OR (aOR) were calculated using multivariate regression models.
Results: Of the 2,573,077 adult hospitalizations with a principal diagnosis of COVID-19, 1.46% (37,670) had been diagnosed with liver cirrhosis. Of these patients, 58.65% were female (p< 0.01), 54.42% were White, 16.27% were African American, and 21.76% were Hispanic (Table 1). Compared to patients without liver cirrhosis, liver cirrhosis was associated with significantly increased mortality (p< 0.01; aOR 1.25), increased risk of ICU admissions (p< 0.01; aOR 1.17), and significantly lower rates of AKI(p< 0.01, aOR 0.81). There was no significant association between liver cirrhosis and mean length of stay(LOS) or mean cost of hospitalisation.
Discussion: Our study shows that in hospitalisations with a principal diagnosis of COVID-19, liver cirrhosis is associated with significantly higher mortality and higher rates of ICU admission, which is comparable to other studies. What is interesting, however, is that there did not appear to be a significant association with mean length of stay or cost of hospitalization. With liver cirrhosis being a major risk factor for poor outcomes in the hospital setting, these findings warrant further investigation to identify how there is no significant difference between mean cost of hospitalization and mean LOS despite higher level of acuity and complexity of care in these patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hameed Ullah indicated no relevant financial relationships.
Mohamad Sharbatji indicated no relevant financial relationships.
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Hasan Raza indicated no relevant financial relationships.
Saeed Ali indicated no relevant financial relationships.
Hameed Ullah, MD1, Mohamad Sharbatji, MD2, Muhammad Jahanzaib Khan, MD3, Hasan Raza, MD4, Saeed Ali, MD5. P1197 - Impact of COVID-19 on Hospitalized Patients With and Without Liver Cirrhosis: Analysis of National Inpatient Sample 2020-2021, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
