Endoscopy Video Forum
Annual Scientific Meeting
Session: Symposium 2C: Endoscopy Video Forum
V1 - The Runaway Bowel: Endoscopic Tethering for Management of a Delayed EUS-Guided Gastroenterostomy Dehiscence
Monday, October 28, 2024
4:50 PM - 5:00 PM ET
Location: Terrace Ballroom 4

Ali Lahooti, BS
Weill Cornell Medicine
New York, NY
Presenting Author - Endoscopy Video Forum(s)
Ali Lahooti, BS1, Anam Rizvi, MD1, Muhammad Usman. Baig, MBBS1, Kate E. Johnson, BS1, SriHari Mahadev, MD2, Kartik Sampath, MD1, David L. Carr-Locke, MA, MD, FACG1, Reem Sharaiha, MD1
1Weill Cornell Medicine, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Malignant gastric outlet obstruction (GOO) leads to diminished quality of life and survival. Endoscopic Ultrasound-guided gastroenterostomy (EUS-GE) is poised to become the preferred treatment for malignant GOO. Delayed complications of the EUS-GE anastomosis are rare. We present a novel case of delayed dehiscence after EUS-GE and its endoscopic management.
Case Description/Methods: A 51-year-old man with metastatic pancreatic adenocarcinoma presented with inability to tolerate oral intake and was found to have malignant GOO on imaging. He underwent EUS-GE with a 15 x 10 mm lumen-apposing-metal stent (LAMS) and an anchoring 7 Fr x 10 cm double-pigtail stent (DPS). Afterwards he reestablished oral intake. 2 weeks later, he decompensated with pneumoperitoneum, dislodgement of LAMS, and large volume ascites on imaging (Figure 1). EGD confirmed dislodgement of the jejunal end of the LAMS and a large peritoneal defect. To seal the perforation a fully covered metal stent (FCMS) was deployed from the jejunum, across the peritoneal defect, through the prior LAMS and into the stomach. The patient stabilized and weaned off pressors. Repeat CT 3 days later showed on-going leak with peritoneal extravasation at the GE anastomosis. Endoscopic intervention was reattempted. After removing FCMS, a double channel endoscope was used to grasp the dehisced jejunal loop in the peritoneum, pulling it back to the stomach, and then jejunal end was resutured to the gastric end of the dehisced anastomosis. A new 20 x 10 mm LAMS was deployed to reestablish the gastroenterostomy. For reinforcement, an anchoring DPS and 2 endoscopic sutures affixed the LAMS to gastric mucosa. No anastomotic leak remained. The patient improved clinically, remained off pressor support without evidence of on-going leak. A few days after the procedure, the patient wished to transition to comfort care without antibiotics or intravenous access and passed shortly thereafter.
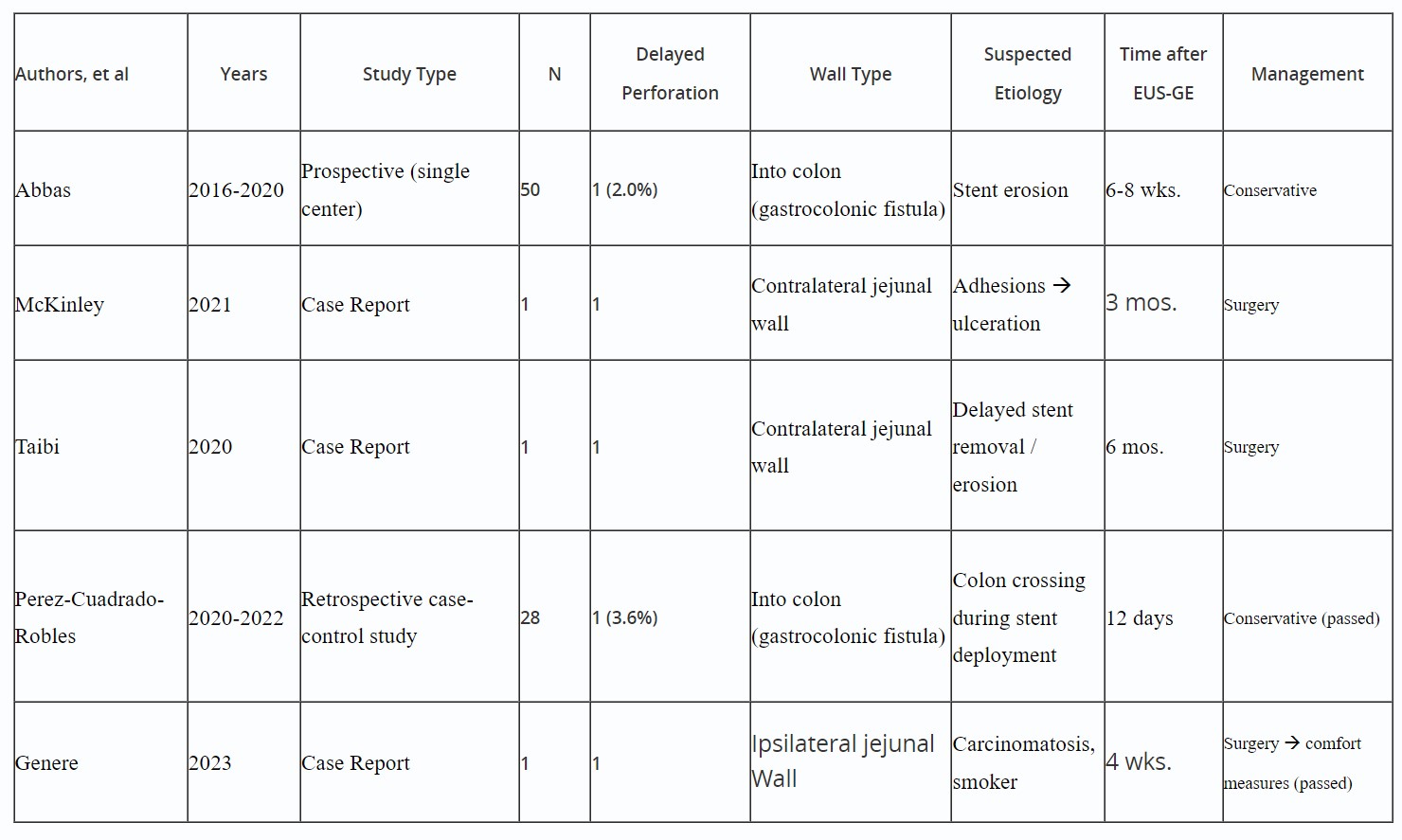
Discussion: Most EUS-GE complications occur in the acute phase and classification systems already exist. Literature shows delayed complications are single case reports of perforations managed surgically or conservatively (Table 1). We demonstrated novel endoscopic management of a delayed EUS-GE dehiscence by endoscopically suturing the anastomotic ends followed by replacement and reinforcement of a LAMS to seal the tract. The clinical durability of this method remains to be validated via future studies.

Disclosures:
Ali Lahooti, BS1, Anam Rizvi, MD1, Muhammad Usman. Baig, MBBS1, Kate E. Johnson, BS1, SriHari Mahadev, MD2, Kartik Sampath, MD1, David L. Carr-Locke, MA, MD, FACG1, Reem Sharaiha, MD1, V1, The Runaway Bowel: Endoscopic Tethering for Management of a Delayed EUS-Guided Gastroenterostomy Dehiscence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Weill Cornell Medicine, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Malignant gastric outlet obstruction (GOO) leads to diminished quality of life and survival. Endoscopic Ultrasound-guided gastroenterostomy (EUS-GE) is poised to become the preferred treatment for malignant GOO. Delayed complications of the EUS-GE anastomosis are rare. We present a novel case of delayed dehiscence after EUS-GE and its endoscopic management.
Case Description/Methods: A 51-year-old man with metastatic pancreatic adenocarcinoma presented with inability to tolerate oral intake and was found to have malignant GOO on imaging. He underwent EUS-GE with a 15 x 10 mm lumen-apposing-metal stent (LAMS) and an anchoring 7 Fr x 10 cm double-pigtail stent (DPS). Afterwards he reestablished oral intake. 2 weeks later, he decompensated with pneumoperitoneum, dislodgement of LAMS, and large volume ascites on imaging (Figure 1). EGD confirmed dislodgement of the jejunal end of the LAMS and a large peritoneal defect. To seal the perforation a fully covered metal stent (FCMS) was deployed from the jejunum, across the peritoneal defect, through the prior LAMS and into the stomach. The patient stabilized and weaned off pressors. Repeat CT 3 days later showed on-going leak with peritoneal extravasation at the GE anastomosis. Endoscopic intervention was reattempted. After removing FCMS, a double channel endoscope was used to grasp the dehisced jejunal loop in the peritoneum, pulling it back to the stomach, and then jejunal end was resutured to the gastric end of the dehisced anastomosis. A new 20 x 10 mm LAMS was deployed to reestablish the gastroenterostomy. For reinforcement, an anchoring DPS and 2 endoscopic sutures affixed the LAMS to gastric mucosa. No anastomotic leak remained. The patient improved clinically, remained off pressor support without evidence of on-going leak. A few days after the procedure, the patient wished to transition to comfort care without antibiotics or intravenous access and passed shortly thereafter.
Discussion: Most EUS-GE complications occur in the acute phase and classification systems already exist. Literature shows delayed complications are single case reports of perforations managed surgically or conservatively (Table 1). We demonstrated novel endoscopic management of a delayed EUS-GE dehiscence by endoscopically suturing the anastomotic ends followed by replacement and reinforcement of a LAMS to seal the tract. The clinical durability of this method remains to be validated via future studies.

Figure: CT scan with oral contrast showing pneumoperitoneum, suspected dislodgment of LAMS from jejunum (cursor) and development of large volume ascites. CT was taken after the patient presented with severe abdominal pain, shock, and cardiac arrest with a clinically concerning picture for perforation.
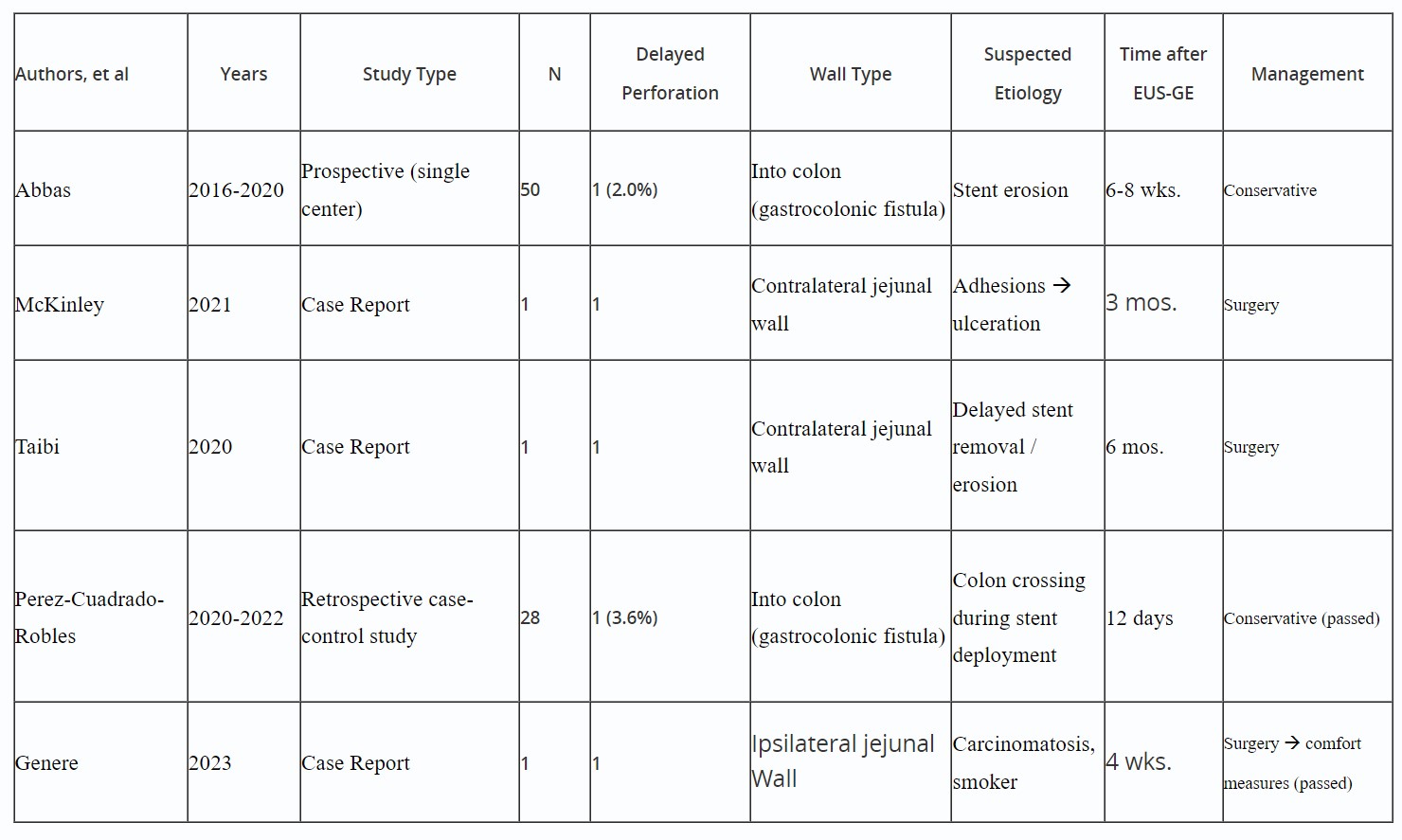
Table: Single case reports showing delayed EUS-GE complication
Disclosures:
Ali Lahooti indicated no relevant financial relationships.
Anam Rizvi indicated no relevant financial relationships.
Muhammad Baig indicated no relevant financial relationships.
Kate Johnson indicated no relevant financial relationships.
SriHari Mahadev: Boston Scientific – Consultant. Conmed – Consultant.
Kartik Sampath indicated no relevant financial relationships.
David Carr-Locke: Steris Corporation – Royalties.
Reem Sharaiha: Boston Scientific – Consultant, Grant/Research Support. Olympus – Consultant. Surgical Intuitive – Advisory Committee/Board Member.
Ali Lahooti, BS1, Anam Rizvi, MD1, Muhammad Usman. Baig, MBBS1, Kate E. Johnson, BS1, SriHari Mahadev, MD2, Kartik Sampath, MD1, David L. Carr-Locke, MA, MD, FACG1, Reem Sharaiha, MD1, V1, The Runaway Bowel: Endoscopic Tethering for Management of a Delayed EUS-Guided Gastroenterostomy Dehiscence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
