Endoscopy Video Forum
Annual Scientific Meeting
Session: Symposium 2C: Endoscopy Video Forum
V3 - Endoscopic Ultrasound-Guided Ileo-Colostomy Creation to Manage Distal Small Bowel Obstruction
Monday, October 28, 2024
5:10 PM - 5:20 PM ET
Location: Terrace Ballroom 4
.jpg)
Brysen Keith, DO, MSBE (he/him/his)
University of Miami Miller School of Medicine
Miami, FL
Presenting Author - Endoscopy Video Forum(s)
Brysen Keith, DO, MSBE1, Shria Kumar, MD, MSCE2, Jodie A. Barkin, MD, FACG3, Sunil Amin, MD, MPH1, Sean Bhalla, MD1
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami, Miami, FL; 3University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: Endoscopic management of proximal malignant small bowel obstructions (SBO) in non-surgical patients with Endoscopic ultrasound (EUS)-guided gastroenterostomy is becoming more common. The endoscopic management of distal malignant SBO is not well established. We present a case of endoscopic management of a malignant distal SBO with EUS-Guided Ileo-colostomy.
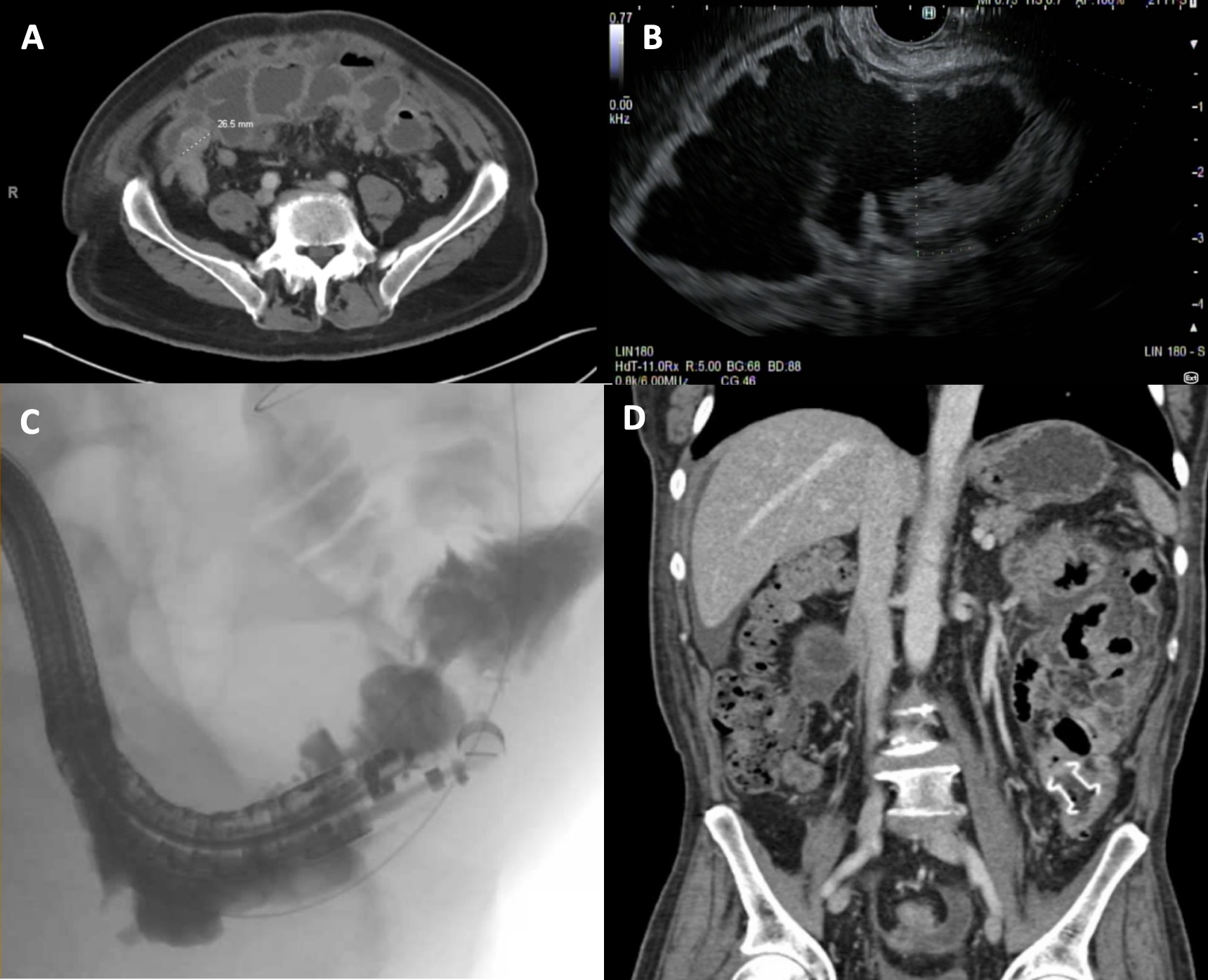
Case Description/Methods: A 73-year-old man with metastatic gallbladder adenocarcinoma on chemotherapy presented with one week of vomiting, abdominal pain, and inability to pass flatus or stool. Computed tomography scan of the abdomen showed a 2.6 cm mass at the terminal ileum causing an SBO. The patient was not a surgical candidate due to his metastatic disease and recent chemotherapy. Endoscopic luminal stenting was considered, however due to the location of obstruction, success would be limited. Venting gastric tube for palliation was discussed, but would not relieve his obstruction. After multidisciplinary discussion with the patient, the decision was made to pursue EUS-guided ileo-colostomy. A colonoscopy with water immersion was then performed to the transverse colon. Under fluoroscopy a 0.035”x 450cm stiff guidewire was advanced into the cecum. The colonoscope was exchanged for the echoendoscope and advanced to the distal descending colon. Dilated loops of small bowel were visualized with the EUS, along with a suitable oblique angle window for creation of an ileo-colostomy. Cautery was applied and a 15 x 10mm lumen apposing metal stent (LAMS) was advanced into the small bowel and deployed. Drainage of fluid and stool was noted. Placement was confirmed with contrast. No signs of bleeding or perforation were noted. The LAMS was then dilated to 8mm. Postoperatively the patient did well, having many loose bowel movements per day and his diet was slowly advanced. Upper GI series on POD 11 showed patent LAMS with passage of contrast and he was later discharged. The patient did well for 14 months post-procedure tolerating PO and continuing chemotherapy. Eventually, 1.5 years later he presented with multiple recurrent SBO’s and a decision was made for hospice.
Discussion: Endoscopic management of distal SBO with EUS-guided Ileo-colostomy is a safe and effective option for non-surgical patients. LAMS placement in distal colon did not lead to clinically significant diarrhea. One year post-procedure follow-up suggests that EUS-guided Ileo-colostomy may be able to provide patients with a durable treatment with improvement in quality of life in comparison to alternative measures.
Disclosures:
Brysen Keith, DO, MSBE1, Shria Kumar, MD, MSCE2, Jodie A. Barkin, MD, FACG3, Sunil Amin, MD, MPH1, Sean Bhalla, MD1, V3, Endoscopic Ultrasound-Guided Ileo-Colostomy Creation to Manage Distal Small Bowel Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami, Miami, FL; 3University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: Endoscopic management of proximal malignant small bowel obstructions (SBO) in non-surgical patients with Endoscopic ultrasound (EUS)-guided gastroenterostomy is becoming more common. The endoscopic management of distal malignant SBO is not well established. We present a case of endoscopic management of a malignant distal SBO with EUS-Guided Ileo-colostomy.
Case Description/Methods: A 73-year-old man with metastatic gallbladder adenocarcinoma on chemotherapy presented with one week of vomiting, abdominal pain, and inability to pass flatus or stool. Computed tomography scan of the abdomen showed a 2.6 cm mass at the terminal ileum causing an SBO. The patient was not a surgical candidate due to his metastatic disease and recent chemotherapy. Endoscopic luminal stenting was considered, however due to the location of obstruction, success would be limited. Venting gastric tube for palliation was discussed, but would not relieve his obstruction. After multidisciplinary discussion with the patient, the decision was made to pursue EUS-guided ileo-colostomy. A colonoscopy with water immersion was then performed to the transverse colon. Under fluoroscopy a 0.035”x 450cm stiff guidewire was advanced into the cecum. The colonoscope was exchanged for the echoendoscope and advanced to the distal descending colon. Dilated loops of small bowel were visualized with the EUS, along with a suitable oblique angle window for creation of an ileo-colostomy. Cautery was applied and a 15 x 10mm lumen apposing metal stent (LAMS) was advanced into the small bowel and deployed. Drainage of fluid and stool was noted. Placement was confirmed with contrast. No signs of bleeding or perforation were noted. The LAMS was then dilated to 8mm. Postoperatively the patient did well, having many loose bowel movements per day and his diet was slowly advanced. Upper GI series on POD 11 showed patent LAMS with passage of contrast and he was later discharged. The patient did well for 14 months post-procedure tolerating PO and continuing chemotherapy. Eventually, 1.5 years later he presented with multiple recurrent SBO’s and a decision was made for hospice.
Discussion: Endoscopic management of distal SBO with EUS-guided Ileo-colostomy is a safe and effective option for non-surgical patients. LAMS placement in distal colon did not lead to clinically significant diarrhea. One year post-procedure follow-up suggests that EUS-guided Ileo-colostomy may be able to provide patients with a durable treatment with improvement in quality of life in comparison to alternative measures.
Figure: Figure A: CT Scan showing 2.6cm mass in the terminal ileum causing a small bowel obstruction. Figure B: Visualization of dilated loops of small bowel using endoscopic ultrasound with oblique angle window for ileo-colostomy creation. Figure C: Contrast injection under fluoroscopy to confirm stent placement. Figure D: CT abdomen and pelvis 1 year post-procedure confirming stent placement and patency.
Disclosures:
Brysen Keith indicated no relevant financial relationships.
Shria Kumar indicated no relevant financial relationships.
Jodie Barkin: Abbvie – Consultant. Aimmune Therapeutics – Consultant. Corevitas – Consultant. Exact Sciences – Consultant. Medtronic – Consultant. Motus GI – Consultant. Organon – Consultant.
Sunil Amin: 3D Matrix – Consultant. Boston Scientific – Consultant. Medtronic – Consultant.
Sean Bhalla indicated no relevant financial relationships.
Brysen Keith, DO, MSBE1, Shria Kumar, MD, MSCE2, Jodie A. Barkin, MD, FACG3, Sunil Amin, MD, MPH1, Sean Bhalla, MD1, V3, Endoscopic Ultrasound-Guided Ileo-Colostomy Creation to Manage Distal Small Bowel Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
