Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2A - Small Intestine / Functional / Liver
27 - Increased Rates of Post-Transplant Diabetes Among Liver Transplant Recipients With Food Insecurity
Tuesday, October 29, 2024
9:50 AM - 10:00 AM ET
Location: Terrace Ballroom 1
Ashley H. Jowell, MD, MS
Duke University School of Medicine
Durham, NC
Presenting Author(s)
Ashley H. Jowell, MD, MS, Jacqueline B. Henson, MD, Andrew J. Muir, MD, MHS
Duke University School of Medicine, Durham, NC
Introduction: Liver transplant (LT) recipients are at risk of post-transplant diabetes (PTDM). We explored the relationship between food insecurity, a known risk factor for diabetes, and PTDM development among LT recipients.
Methods: First-time LT recipients from 7/2004-12/2022 without diabetes and with ≥ 1 year of follow-up were identified in the UNOS SRTR database. Data from the USDA Food Environment Atlas and County Health Rankings on three measures of healthy food access at the county level were obtained: population with food insecurity, low-income population with low access to grocery stores (food deserts), and ratio of unhealthy to healthy food options (food swamps), all expressed by quartile. The primary endpoint was PTDM development; secondary endpoints were all-cause mortality and death due to cardiovascular disease (CVD) or infection. Competing risks analysis was performed to account for the competing risk of death in developing PTDM and for other causes of death for cause-specific mortality. Multivariable analyses were used to adjust for demographic and clinical factors.
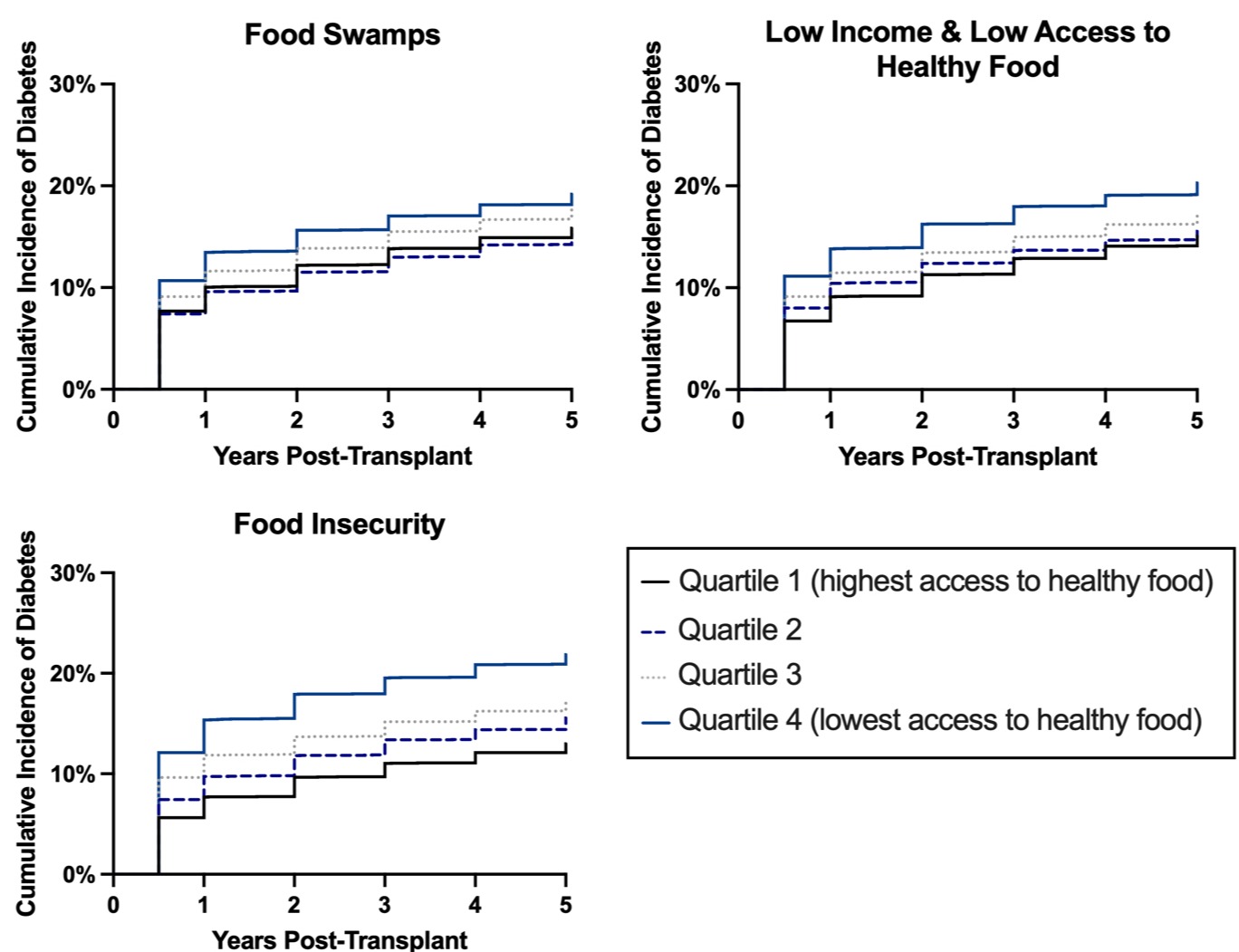
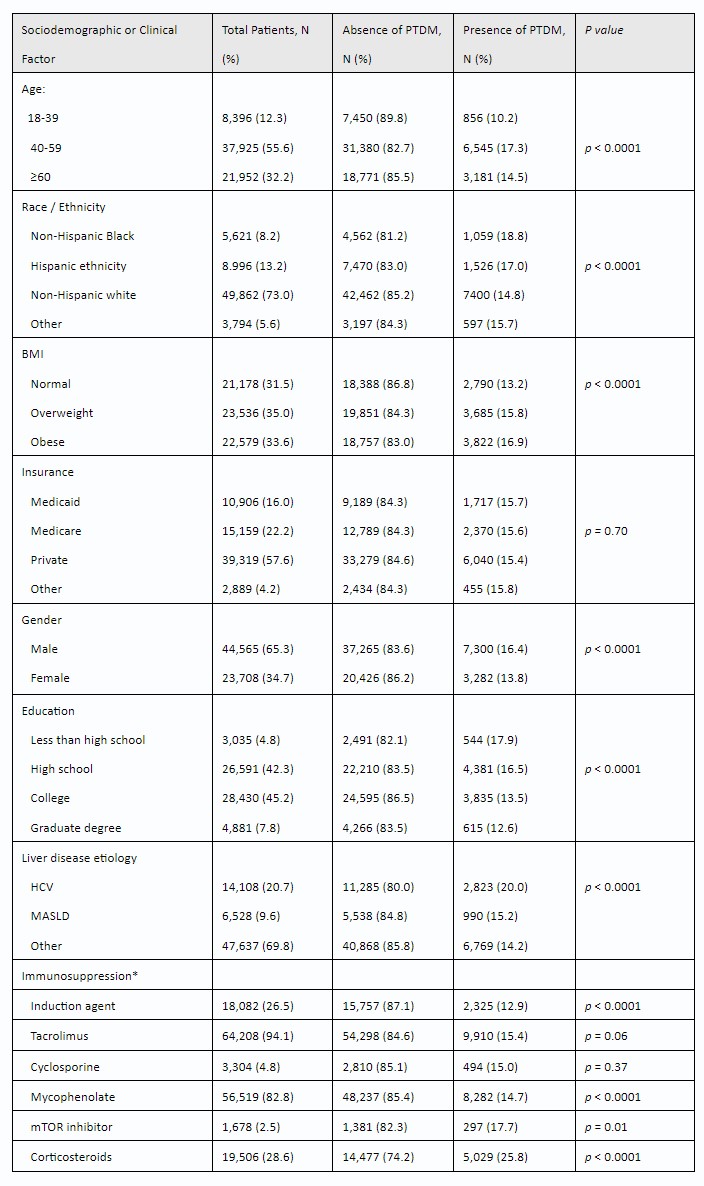
Results: 68,273 LT recipients met inclusion criteria; 15.5% developed PTDM (Table). The proportion who developed PTDM was nearly twice as high in counties with the greatest food insecurity vs. the lowest (21% vs. 11%, p < 0.001; Figure). Similarly, patients in counties with the greatest population in food deserts and in the greatest food swamps were more likely to develop PTDM (19% vs. 13%, p < 0.001 and 18% vs. 14%, p < 0.001, respectively; Figure). This relationship persisted when adjusting for PTDM risk factors (highest vs. lowest quartile food insecurity: subhazard ratio [sHR] 1.58, 95% confidence interval [CI] 1.46-1.71; food deserts: sHR 1.42, 95% CI 1.34-1.51; food swamps: sHR 1.26, 95% CI 1.20-1.34). PTDM risk was higher among patients prescribed steroids at six months post LT (25.8% vs. 11.4%, p < 0.001). PTDM was associated with all-cause post LT mortality (sHR 1.18, 95% CI 1.13-1.22), CVD mortality (sHR 1.19, 95% CI 1.04-1.35), and mortality due to infection (sHR 1.29, 95% CI 1.13-1.48).
Discussion: In this national cohort study, LT recipients in counties with decreased access to healthy foods were more likely to develop PTDM and patients with PTDM had increased mortality. Our findings underscore the importance of screening for food insecurity, a modifiable social determinant of health, among LT recipients. Future work should assess the impact of interventions increasing access to healthy foods on these outcomes.
Disclosures:
Ashley H. Jowell, MD, MS, Jacqueline B. Henson, MD, Andrew J. Muir, MD, MHS, 27, Increased Rates of Post-Transplant Diabetes Among Liver Transplant Recipients With Food Insecurity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Duke University School of Medicine, Durham, NC
Introduction: Liver transplant (LT) recipients are at risk of post-transplant diabetes (PTDM). We explored the relationship between food insecurity, a known risk factor for diabetes, and PTDM development among LT recipients.
Methods: First-time LT recipients from 7/2004-12/2022 without diabetes and with ≥ 1 year of follow-up were identified in the UNOS SRTR database. Data from the USDA Food Environment Atlas and County Health Rankings on three measures of healthy food access at the county level were obtained: population with food insecurity, low-income population with low access to grocery stores (food deserts), and ratio of unhealthy to healthy food options (food swamps), all expressed by quartile. The primary endpoint was PTDM development; secondary endpoints were all-cause mortality and death due to cardiovascular disease (CVD) or infection. Competing risks analysis was performed to account for the competing risk of death in developing PTDM and for other causes of death for cause-specific mortality. Multivariable analyses were used to adjust for demographic and clinical factors.
Results: 68,273 LT recipients met inclusion criteria; 15.5% developed PTDM (Table). The proportion who developed PTDM was nearly twice as high in counties with the greatest food insecurity vs. the lowest (21% vs. 11%, p < 0.001; Figure). Similarly, patients in counties with the greatest population in food deserts and in the greatest food swamps were more likely to develop PTDM (19% vs. 13%, p < 0.001 and 18% vs. 14%, p < 0.001, respectively; Figure). This relationship persisted when adjusting for PTDM risk factors (highest vs. lowest quartile food insecurity: subhazard ratio [sHR] 1.58, 95% confidence interval [CI] 1.46-1.71; food deserts: sHR 1.42, 95% CI 1.34-1.51; food swamps: sHR 1.26, 95% CI 1.20-1.34). PTDM risk was higher among patients prescribed steroids at six months post LT (25.8% vs. 11.4%, p < 0.001). PTDM was associated with all-cause post LT mortality (sHR 1.18, 95% CI 1.13-1.22), CVD mortality (sHR 1.19, 95% CI 1.04-1.35), and mortality due to infection (sHR 1.29, 95% CI 1.13-1.48).
Discussion: In this national cohort study, LT recipients in counties with decreased access to healthy foods were more likely to develop PTDM and patients with PTDM had increased mortality. Our findings underscore the importance of screening for food insecurity, a modifiable social determinant of health, among LT recipients. Future work should assess the impact of interventions increasing access to healthy foods on these outcomes.
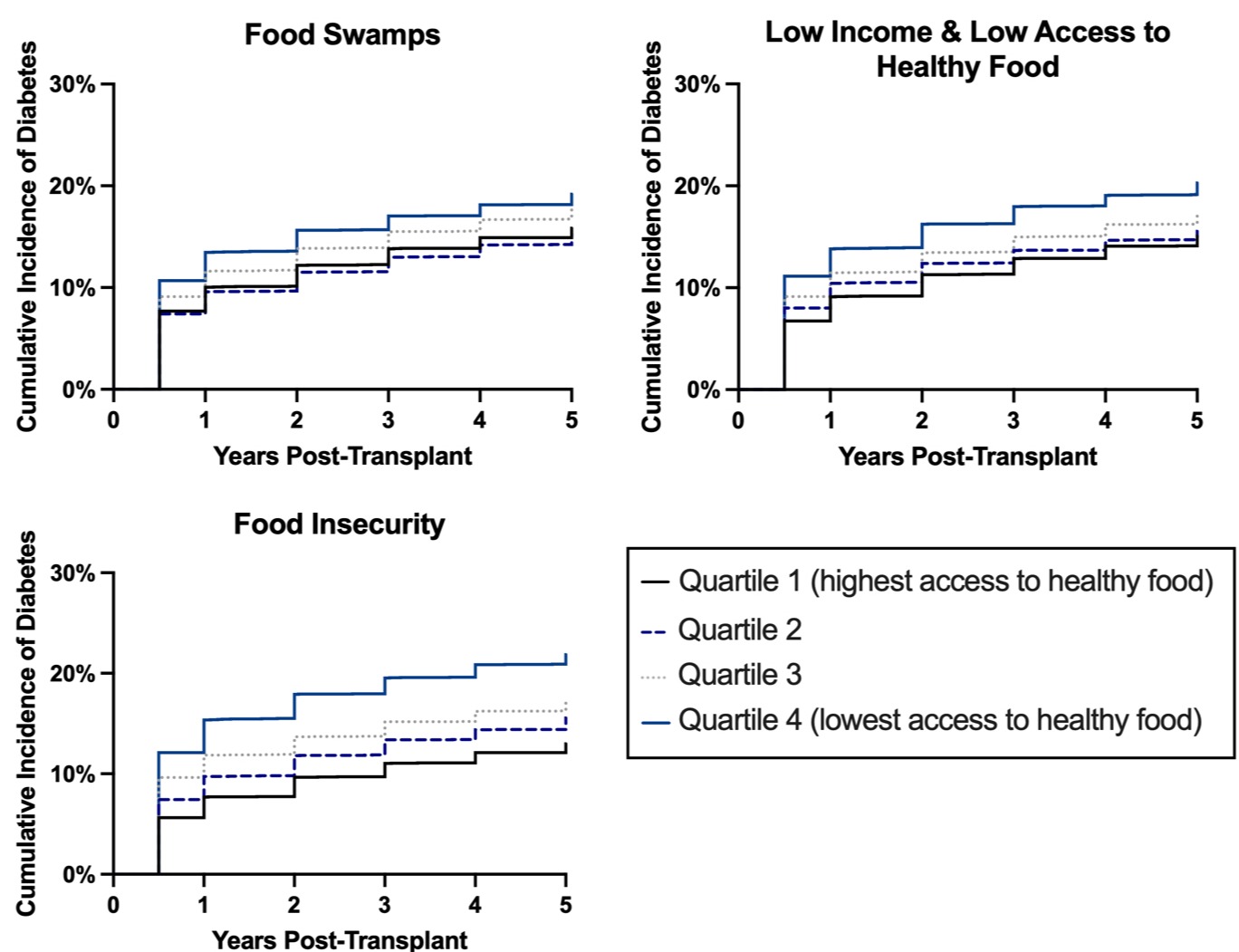
Figure: Figure 1: Time free of post-transplant diabetes, by measures of access to healthy food
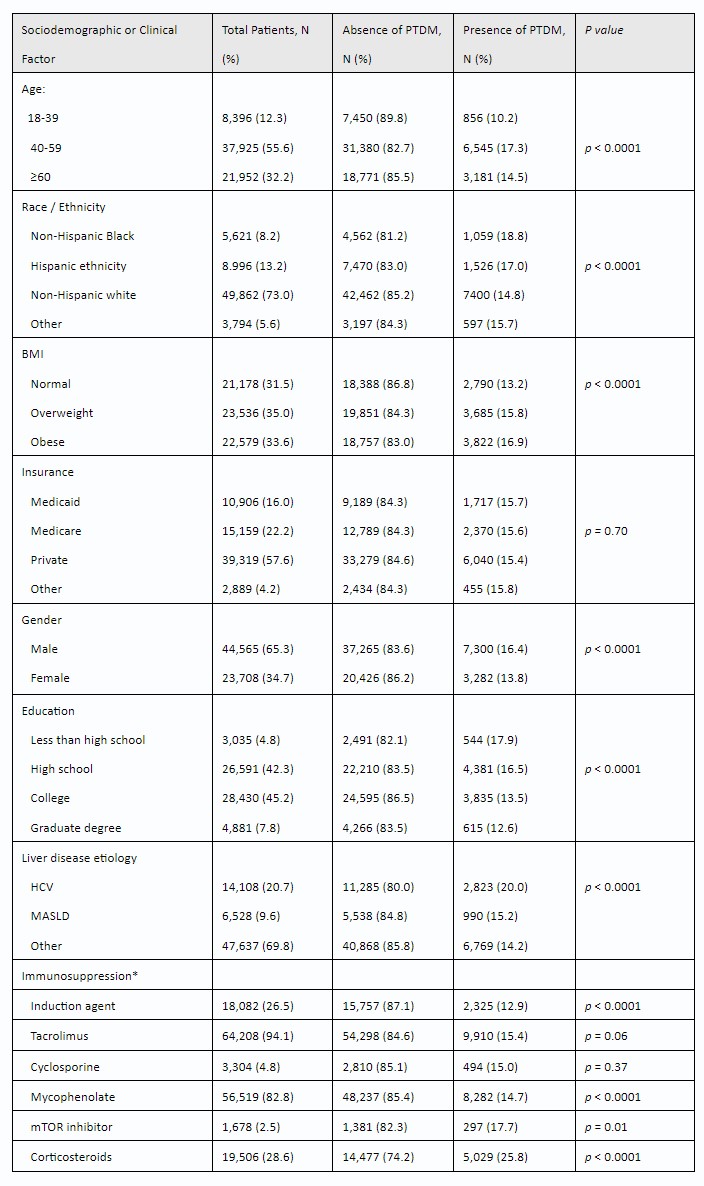
Table: Table 1: Risk of New Onset Post-Transplant Diabetes (PTDM) and Sociodemographic Factors.
*Regimen at discharge with exception of corticosteroids, which was assessed at 6 months.
*Regimen at discharge with exception of corticosteroids, which was assessed at 6 months.
Disclosures:
Ashley Jowell indicated no relevant financial relationships.
Jacqueline Henson indicated no relevant financial relationships.
Andrew Muir indicated no relevant financial relationships.
Ashley H. Jowell, MD, MS, Jacqueline B. Henson, MD, Andrew J. Muir, MD, MHS, 27, Increased Rates of Post-Transplant Diabetes Among Liver Transplant Recipients With Food Insecurity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

