Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 4B - IBD
66 - Major Adverse Cardiovascular Events in Patients With IBD Taking Anti-TNF vs JAK Inhibitors: A Propensity Matched Cohort Analysis
Wednesday, October 30, 2024
8:40 AM - 8:50 AM ET
Location: Terrace Ballroom 2-3
.jpg)
Saqr Alsakarneh, MD (he/him/his)
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Saqr Alsakarneh, MD1, Mahmoud Madi, MD2, Fouad Jaber, MD1, Francis A. Farraye, MD, MSc3, Adam S.. Faye, MD4, Freddy Caldera, DO, PhD5
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Saint Louis University School of Medicine, St. Louis, MO; 3Mayo Clinic, Jacksonville, FL; 4NYU Grossman School of Medicine, New York, NY; 5University of Wisconsin School of Medicine and Public Health, MIddleton, WI
Introduction: Inflammatory bowel disease (IBD) is associated with an increased risk of major adverse cardiovascular events (MACE). Janus kinase inhibitors (JAKi) are approved to treat IBD, but there are concerns over whether they increase the risk of MACE or venous thromboembolism (VTE) in patients with IBD. We aimed to compare the incident risk of MACE and VTE in IBD patients treated with anti-TNF agents versus JAKi.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify patients ≥18 years with IBD and treated with JAK inhibitors or anti-TNF therapy. Patients in the JAKi cohort were matched with patients treated with anti-TNF by using 1:1 propensity score matching. Patients with a history of a prior cardiovascular event were excluded from the analysis. Co-primary outcomes were MACE and VTE within 1-year after medication initiation. Additional subgroup analyses were performed based on age, sex, and IBD type. Kaplan-Meier analysis with adjusted hazard ratios (HRs) and 95% CIs were used to compare time to event rates.
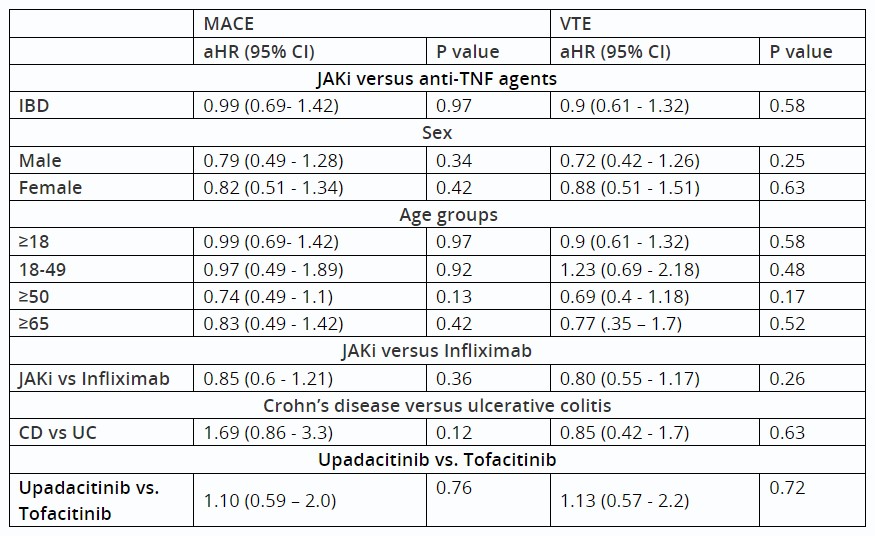
Results: In total, there were 3,740 patients in the JAKi cohort (mean age 43.1 years, 48.9% female, 75.3% White) matched with 3,740 patients in the anti-TNF cohort (mean age 43.0 years, 48.9% female, 75.3% White). After excluding patients with a history of prior cardiovascular events, 57 (1.76%) of the JAKi cohort developed MACE events versus 63 (1.94%) in the anti-TNF cohort. There was no difference between the two cohorts in the development of MACE (aHR: 0.99; 95% CI: 0.69 - 1.42) or VTE (aHR: 0.9; 95% CI: 0.61 - 1.32). In patients aged ≥65 years, 25 (5.3%) patients had MACE events in the JAKi cohort versus 30 (6.4%) in the anti-TNF cohort with no statistically significant difference (aHR = 0.83; 95% CI: 0.49 – 1.42). While patients in the JAKi cohort were more likely to undergo intestinal resection surgery (aHR: 1.32; 95% CI: 0.1.06 – 1.64), there was no statistically significant difference in terms of systematic corticosteroids use (aHR: 0.99; 95% CI: 0.92 – 1.05). There was no difference on subgroup analysis when comparing ulcerative colitis to Crohn’s disease, upadacitinib to tofacitinib, or JAKi to infliximab.
Discussion: Our results suggest that patients with IBD, including older patients, who are treated with JAKi were not at increased risk of MACE or VTE over a twelve-month period as compared to those treated with anti-TNF therapy. Further prospective studies are warranted to confirm these findings.
Disclosures:
Saqr Alsakarneh, MD1, Mahmoud Madi, MD2, Fouad Jaber, MD1, Francis A. Farraye, MD, MSc3, Adam S.. Faye, MD4, Freddy Caldera, DO, PhD5, 66, Major Adverse Cardiovascular Events in Patients With IBD Taking Anti-TNF vs JAK Inhibitors: A Propensity Matched Cohort Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Saint Louis University School of Medicine, St. Louis, MO; 3Mayo Clinic, Jacksonville, FL; 4NYU Grossman School of Medicine, New York, NY; 5University of Wisconsin School of Medicine and Public Health, MIddleton, WI
Introduction: Inflammatory bowel disease (IBD) is associated with an increased risk of major adverse cardiovascular events (MACE). Janus kinase inhibitors (JAKi) are approved to treat IBD, but there are concerns over whether they increase the risk of MACE or venous thromboembolism (VTE) in patients with IBD. We aimed to compare the incident risk of MACE and VTE in IBD patients treated with anti-TNF agents versus JAKi.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify patients ≥18 years with IBD and treated with JAK inhibitors or anti-TNF therapy. Patients in the JAKi cohort were matched with patients treated with anti-TNF by using 1:1 propensity score matching. Patients with a history of a prior cardiovascular event were excluded from the analysis. Co-primary outcomes were MACE and VTE within 1-year after medication initiation. Additional subgroup analyses were performed based on age, sex, and IBD type. Kaplan-Meier analysis with adjusted hazard ratios (HRs) and 95% CIs were used to compare time to event rates.
Results: In total, there were 3,740 patients in the JAKi cohort (mean age 43.1 years, 48.9% female, 75.3% White) matched with 3,740 patients in the anti-TNF cohort (mean age 43.0 years, 48.9% female, 75.3% White). After excluding patients with a history of prior cardiovascular events, 57 (1.76%) of the JAKi cohort developed MACE events versus 63 (1.94%) in the anti-TNF cohort. There was no difference between the two cohorts in the development of MACE (aHR: 0.99; 95% CI: 0.69 - 1.42) or VTE (aHR: 0.9; 95% CI: 0.61 - 1.32). In patients aged ≥65 years, 25 (5.3%) patients had MACE events in the JAKi cohort versus 30 (6.4%) in the anti-TNF cohort with no statistically significant difference (aHR = 0.83; 95% CI: 0.49 – 1.42). While patients in the JAKi cohort were more likely to undergo intestinal resection surgery (aHR: 1.32; 95% CI: 0.1.06 – 1.64), there was no statistically significant difference in terms of systematic corticosteroids use (aHR: 0.99; 95% CI: 0.92 – 1.05). There was no difference on subgroup analysis when comparing ulcerative colitis to Crohn’s disease, upadacitinib to tofacitinib, or JAKi to infliximab.
Discussion: Our results suggest that patients with IBD, including older patients, who are treated with JAKi were not at increased risk of MACE or VTE over a twelve-month period as compared to those treated with anti-TNF therapy. Further prospective studies are warranted to confirm these findings.
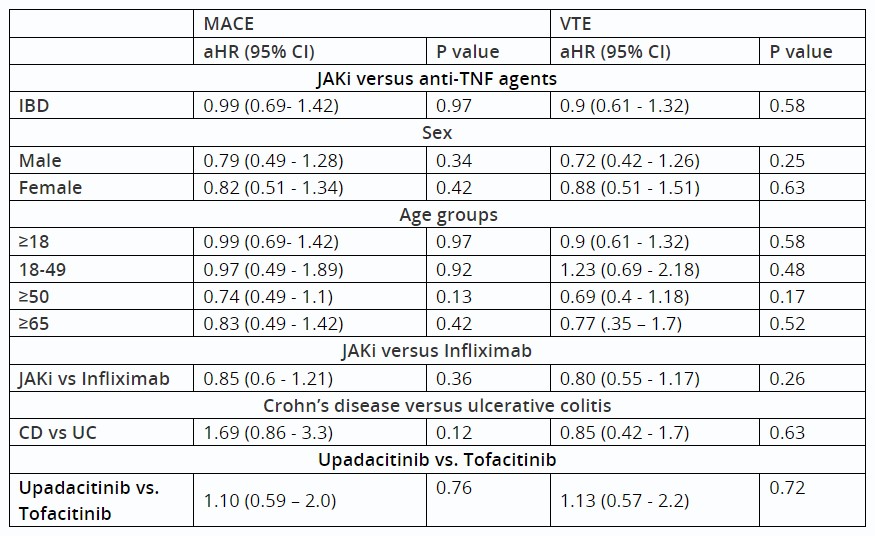
Table: Table 1: Comparison of MACE and VTE risk between patients with inflammatory bowel disease treated with JAK inhibitors versus anti-TNF agents.
Abbreviations: aHR: Adjusted hazardous ratio; IBD: Inflammatory bowel disease; JAKi: Janus Kinase inhibitors; anti-TNF: Anit-Tumor necrosis factor; MACE: Major adverse cardiovascular events; VTE: Venous thromboembolism.
Abbreviations: aHR: Adjusted hazardous ratio; IBD: Inflammatory bowel disease; JAKi: Janus Kinase inhibitors; anti-TNF: Anit-Tumor necrosis factor; MACE: Major adverse cardiovascular events; VTE: Venous thromboembolism.
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Fouad Jaber indicated no relevant financial relationships.
Francis Farraye: AbbVie – Consultant. Avalo Therapeutics – Consultant. Bausch – Advisor or Review Panel Member. BMS – Consultant. Braintree Labs – Consultant. DSMB for Lilly. – Sits on. Fresenius Kabi – Consultant. GI Reviewers and IBD Educational Group – independent contractor. GSK, Iterative Health, Janssen, Pfizer, Pharmacosmos, Sandoz Immunology, Sebela and Viatris – Consultant.
Adam Faye: Abbvie – Consultant. BMS – Consultant. Takeda – Education Seminar.
Freddy Caldera: GSK – Consultant. GSK – Grant/Research Support. Janssen – Advisory Committee/Board Member. Janssen – Consultant. Novavax – Grant/Research Support.
Saqr Alsakarneh, MD1, Mahmoud Madi, MD2, Fouad Jaber, MD1, Francis A. Farraye, MD, MSc3, Adam S.. Faye, MD4, Freddy Caldera, DO, PhD5, 66, Major Adverse Cardiovascular Events in Patients With IBD Taking Anti-TNF vs JAK Inhibitors: A Propensity Matched Cohort Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.



