Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 4A - Liver
57 - Monitoring Gaps and Treatment Disparities Among Adults With Chronic Hepatitis B Infection in the United States: Role of Treatment Eligibility Criteria
Wednesday, October 30, 2024
8:50 AM - 9:00 AM ET
Location: Terrace Ballroom 1

Robert Wong, MD, MS, FACG
Stanford/VA Palo Alto
Palo Alto, CA
Presenting Author(s)
Robert Wong, MD, MS, FACG1, George Therapondos, MD2, Mamta K.. Jain, MD3, Bolin Niu, MD4, Onkar Kshirsagar, MS5, MAE THAMER, PhD6
1Stanford/VA Palo Alto, Palo Alto, CA; 2Ochsner Health System, New Orleans, LA; 3UT Southwestern Medical Center, Dallas, TX; 4Case Western Reserve University / MetroHealth, Cleveland, OH; 5MTPPI, Bethesda, MD; 6MTPPI, Potomac, MD
Introduction: Gaps in treatment of chronic hepatitis B (CHB) patients persist and may in part be influenced by complex criteria for assessing treatment eligibility (TxElig). Calls for simplifying CHB treatment criteria are growing; recently Dieterich et al (Gastro Hep Adv 2023;2:209-18) proposed a Simplified Approach to Hepatitis B Algorithm (SABA), recommending simplifying treatment of non-cirrhotic CHB patients who are 1) age>30y and HBV DNA >2000 IU/mL, regardless of alanine aminotransferase (ALT) level, or 2) age< 30y with HBV DNA >2000 IU/mL and ALT > 30 IU/mL in men ( >19 IU/ml in women). We aim to evaluate gaps and disparities in CHB treatment among an ethnically diverse cohort of CHB patients using established AASLD criteria and modeling the impact of applying newly proposed SABA criteria.
Methods: Adults with treatment-naïve CHB identified from 2010 to 2018 across 3 safety-net health systems were evaluated for TxElig based on AASLD CHB guidelines and recently proposed SABA criteria. HIV co-infected patients were excluded. Among TxElig patients, proportions that received CHB treatment between groups were compared using chi-square methods. Adjusted Cox proportional hazards models evaluated for predictors of CHB treatment among TxElig patients.
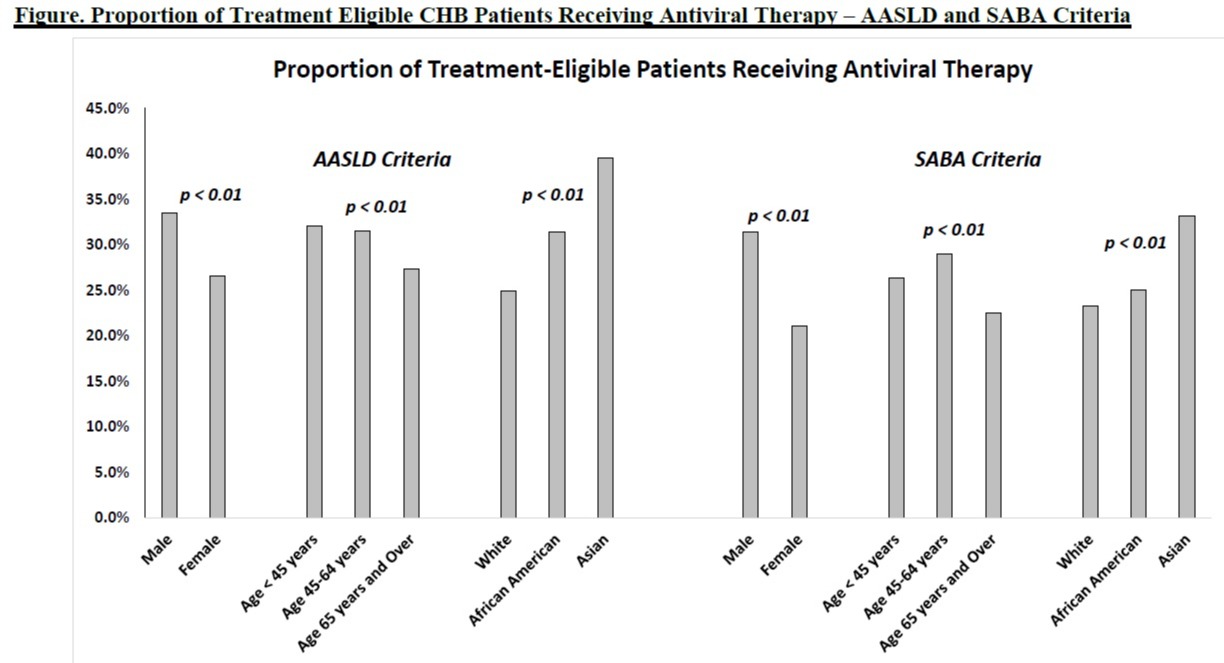
Results: Among 3,749 CHB patients (51.5% women, 38.7% white, 33.7% African American, 19.6% Asian, 24.6% with cirrhosis), 30.0% (n=1,126) were AASLD TxElig and 45.3% (n=1,698) were SABA TxElig. Among AASLD TxElig patients, unadjusted univariate analyses demonstrated higher rates of receiving CHB treatment in men vs. women, in younger patients age < 45y vs. age >65y, and in Asians vs. whites (Figure). On regression analyses, only race/ethnicity-specific differences persisted with Asians more likely to be treated than whites (aHR 1.55, 95% CI 1.14-2.11, p< 0.01). Among SABA TxElig patients, similar trends were seen; higher rates of CHB treatment were observed in men vs. women, Asians vs. whites, and in younger patients (Figure). On regression analyses, both gender and race/ethnicity differences persisted: men vs. women (aHR 1.40, 95% CI 1.14-1.70, p< 0.01) and Asians vs. whites (aHR 1.50, 95% CI 1.16-1.94, p< 0.01).
Discussion: Among a predominantly non-Asian cohort of CHB patients, less than one-third of AASLD TxElig patients received CHB treatment. When applying simplified SABA criteria, over 45% became treatment-eligible, but major gaps in actually receiving treatment persisted, especially among non-Asians and women.
Disclosures:
Robert Wong, MD, MS, FACG1, George Therapondos, MD2, Mamta K.. Jain, MD3, Bolin Niu, MD4, Onkar Kshirsagar, MS5, MAE THAMER, PhD6, 57, Monitoring Gaps and Treatment Disparities Among Adults With Chronic Hepatitis B Infection in the United States: Role of Treatment Eligibility Criteria, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Stanford/VA Palo Alto, Palo Alto, CA; 2Ochsner Health System, New Orleans, LA; 3UT Southwestern Medical Center, Dallas, TX; 4Case Western Reserve University / MetroHealth, Cleveland, OH; 5MTPPI, Bethesda, MD; 6MTPPI, Potomac, MD
Introduction: Gaps in treatment of chronic hepatitis B (CHB) patients persist and may in part be influenced by complex criteria for assessing treatment eligibility (TxElig). Calls for simplifying CHB treatment criteria are growing; recently Dieterich et al (Gastro Hep Adv 2023;2:209-18) proposed a Simplified Approach to Hepatitis B Algorithm (SABA), recommending simplifying treatment of non-cirrhotic CHB patients who are 1) age>30y and HBV DNA >2000 IU/mL, regardless of alanine aminotransferase (ALT) level, or 2) age< 30y with HBV DNA >2000 IU/mL and ALT > 30 IU/mL in men ( >19 IU/ml in women). We aim to evaluate gaps and disparities in CHB treatment among an ethnically diverse cohort of CHB patients using established AASLD criteria and modeling the impact of applying newly proposed SABA criteria.
Methods: Adults with treatment-naïve CHB identified from 2010 to 2018 across 3 safety-net health systems were evaluated for TxElig based on AASLD CHB guidelines and recently proposed SABA criteria. HIV co-infected patients were excluded. Among TxElig patients, proportions that received CHB treatment between groups were compared using chi-square methods. Adjusted Cox proportional hazards models evaluated for predictors of CHB treatment among TxElig patients.
Results: Among 3,749 CHB patients (51.5% women, 38.7% white, 33.7% African American, 19.6% Asian, 24.6% with cirrhosis), 30.0% (n=1,126) were AASLD TxElig and 45.3% (n=1,698) were SABA TxElig. Among AASLD TxElig patients, unadjusted univariate analyses demonstrated higher rates of receiving CHB treatment in men vs. women, in younger patients age < 45y vs. age >65y, and in Asians vs. whites (Figure). On regression analyses, only race/ethnicity-specific differences persisted with Asians more likely to be treated than whites (aHR 1.55, 95% CI 1.14-2.11, p< 0.01). Among SABA TxElig patients, similar trends were seen; higher rates of CHB treatment were observed in men vs. women, Asians vs. whites, and in younger patients (Figure). On regression analyses, both gender and race/ethnicity differences persisted: men vs. women (aHR 1.40, 95% CI 1.14-1.70, p< 0.01) and Asians vs. whites (aHR 1.50, 95% CI 1.16-1.94, p< 0.01).
Discussion: Among a predominantly non-Asian cohort of CHB patients, less than one-third of AASLD TxElig patients received CHB treatment. When applying simplified SABA criteria, over 45% became treatment-eligible, but major gaps in actually receiving treatment persisted, especially among non-Asians and women.
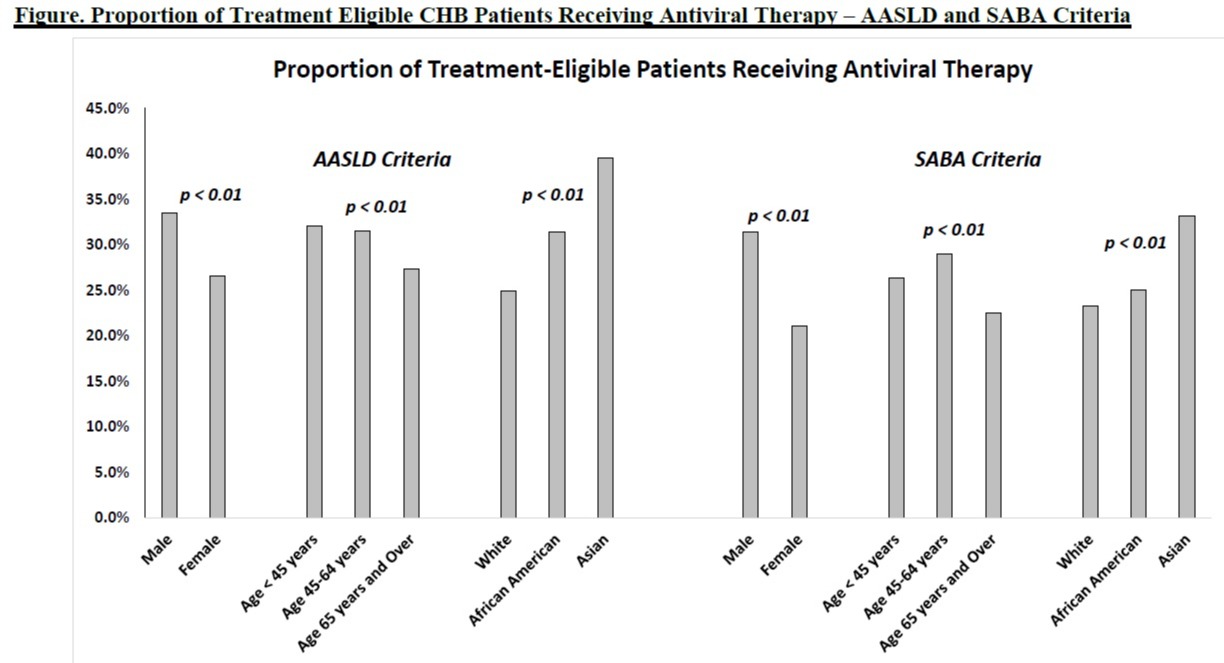
Figure: Proportion of Treatment Eligible CHB Patients Receiving Antiviral Therapy – AASLD and SABA Criteria
Disclosures:
Robert Wong: Durect Corporation – Grant/Research Support. Exact Sciences – Grant/Research Support. Gilead Sciences – Grant/Research Support. Thera Technologies – Grant/Research Support.
George Therapondos indicated no relevant financial relationships.
Mamta Jain: Abbvie – Grant/Research Support. Gilead Sciences – Grant/Research Support. Laurent – Grant/Research Support.
Bolin Niu indicated no relevant financial relationships.
Onkar Kshirsagar indicated no relevant financial relationships.
MAE THAMER: Gilead Sciences – Grant/Research Support.
Robert Wong, MD, MS, FACG1, George Therapondos, MD2, Mamta K.. Jain, MD3, Bolin Niu, MD4, Onkar Kshirsagar, MS5, MAE THAMER, PhD6, 57, Monitoring Gaps and Treatment Disparities Among Adults With Chronic Hepatitis B Infection in the United States: Role of Treatment Eligibility Criteria, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

