Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 4B - IBD
67 - Impact of Gender-Affirming Hormone Therapy in Transgender and Gender Non-Conforming Patients With Inflammatory Bowel Disease
Wednesday, October 30, 2024
8:50 AM - 9:00 AM ET
Location: Terrace Ballroom 2-3

Audrey Bennett, MD (she/her/hers)
Vanderbilt University Medical Center
Nashville, TN
Presenting Author(s)
Austin Lin, MD1, Jenna Davison, MD, MPH2, Shravya Pothula, MD3, Justin Field, MD4, Kira L. Newman, MD, PhD1, Sara N. Horst, MD5, Benjamin Click, MD3, Victor Chedid, MD, MS2, Audrey Bennett, MD6
1University of Michigan, Ann Arbor, MI; 2Mayo Clinic, Rochester, MN; 3University of Colorado, Aurora, CO; 4University of California San Francisco, San Francisco, CA; 5Vanderbilt Inflammatory Bowel Disease Clinic, Nashville, TN; 6Vanderbilt University Medical Center, Nashville, TN
Introduction: Little is known about inflammatory bowel disease (IBD) outcomes in transgender and gender non-conforming (TGNC) patients (pts) or the impact of gender-affirming hormone (GAH) therapy. The aim of this study was to evaluate rate of IBD flare after GAH initiation.
Methods: This was an IRB approved, retrospective, multicenter study across five tertiary care IBD centers. Adult TGNC pts with IBD were identified through the electronic medical record by use of demographic data (including self-reported gender identity where available) and ICD-10 diagnoses. Records were reviewed for clinical characteristics and outcomes. IBD flare was defined as new steroid prescription, IBD-associated emergency department visit, or need for IBD medication change. Factors associated with IBD flare were assessed with univariate analysis (Pearson Chi square) and multivariable logistic regression controlling for age (< 30 or ≥30 years of age), disease type, hormone type, advanced IBD therapy, and disease status at GAH initiation. Disease status was based on a combination of patient reported IBD symptoms, inflammatory markers, and colonoscopy results if performed within six months of GAH start.
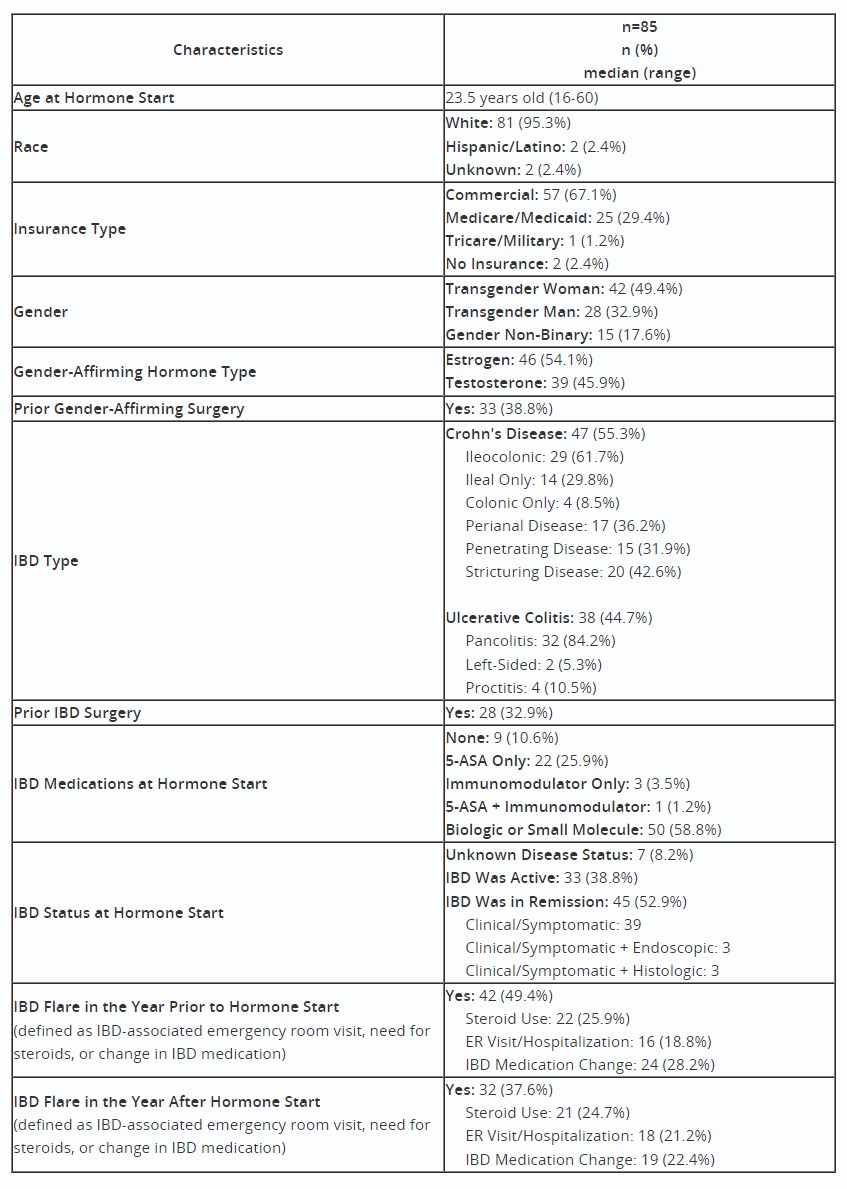
Results: 85 TGNC pts who received GAH therapy were included. 46 trans women (54.1%) received GAH with estrogen and 39 trans men (45.9%) received GAH with testosterone. Table 1 details clinical characteristics. In the year prior to GAH therapy, 42 pts (49%) flared compared to 32 pts (38%) in the year after GAH start (p=0.06). There was no statistically significant difference for flare after GAH initiation among age (< 30: 42% vs ≥30: 30%, p=0.26), IBD type (UC: 30% vs CD: 45%, p=0.19), or use of advanced IBD therapy (no: 34% vs yes: 40%, p=0.59). Pts with active IBD symptoms at GAH initiation were more likely to flare in univariate (58% vs 24%, p=0.003) and multivariable modeling (OR 5.1 [95% CI 1.7 – 15.2]). Trans men initiating testosterone were more likely to flare after GAH initiation compared to trans women initiating estrogen in univariate (trans men: 51% vs trans women: 26%, p=0.02) and multivariable modeling (OR 3.1 [95% CI 1.2 – 8.1]).
Discussion: This study found no overall increased risk of IBD flare in the year after GAH start. Patients with active IBD prior to GAH initiation were more likely to experience an IBD flare in the year after GAH start. Further prospective evaluation on the influence of hormone therapy on disease outcomes is needed.
Disclosures:
Austin Lin, MD1, Jenna Davison, MD, MPH2, Shravya Pothula, MD3, Justin Field, MD4, Kira L. Newman, MD, PhD1, Sara N. Horst, MD5, Benjamin Click, MD3, Victor Chedid, MD, MS2, Audrey Bennett, MD6, 67, Impact of Gender-Affirming Hormone Therapy in Transgender and Gender Non-Conforming Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2Mayo Clinic, Rochester, MN; 3University of Colorado, Aurora, CO; 4University of California San Francisco, San Francisco, CA; 5Vanderbilt Inflammatory Bowel Disease Clinic, Nashville, TN; 6Vanderbilt University Medical Center, Nashville, TN
Introduction: Little is known about inflammatory bowel disease (IBD) outcomes in transgender and gender non-conforming (TGNC) patients (pts) or the impact of gender-affirming hormone (GAH) therapy. The aim of this study was to evaluate rate of IBD flare after GAH initiation.
Methods: This was an IRB approved, retrospective, multicenter study across five tertiary care IBD centers. Adult TGNC pts with IBD were identified through the electronic medical record by use of demographic data (including self-reported gender identity where available) and ICD-10 diagnoses. Records were reviewed for clinical characteristics and outcomes. IBD flare was defined as new steroid prescription, IBD-associated emergency department visit, or need for IBD medication change. Factors associated with IBD flare were assessed with univariate analysis (Pearson Chi square) and multivariable logistic regression controlling for age (< 30 or ≥30 years of age), disease type, hormone type, advanced IBD therapy, and disease status at GAH initiation. Disease status was based on a combination of patient reported IBD symptoms, inflammatory markers, and colonoscopy results if performed within six months of GAH start.
Results: 85 TGNC pts who received GAH therapy were included. 46 trans women (54.1%) received GAH with estrogen and 39 trans men (45.9%) received GAH with testosterone. Table 1 details clinical characteristics. In the year prior to GAH therapy, 42 pts (49%) flared compared to 32 pts (38%) in the year after GAH start (p=0.06). There was no statistically significant difference for flare after GAH initiation among age (< 30: 42% vs ≥30: 30%, p=0.26), IBD type (UC: 30% vs CD: 45%, p=0.19), or use of advanced IBD therapy (no: 34% vs yes: 40%, p=0.59). Pts with active IBD symptoms at GAH initiation were more likely to flare in univariate (58% vs 24%, p=0.003) and multivariable modeling (OR 5.1 [95% CI 1.7 – 15.2]). Trans men initiating testosterone were more likely to flare after GAH initiation compared to trans women initiating estrogen in univariate (trans men: 51% vs trans women: 26%, p=0.02) and multivariable modeling (OR 3.1 [95% CI 1.2 – 8.1]).
Discussion: This study found no overall increased risk of IBD flare in the year after GAH start. Patients with active IBD prior to GAH initiation were more likely to experience an IBD flare in the year after GAH start. Further prospective evaluation on the influence of hormone therapy on disease outcomes is needed.
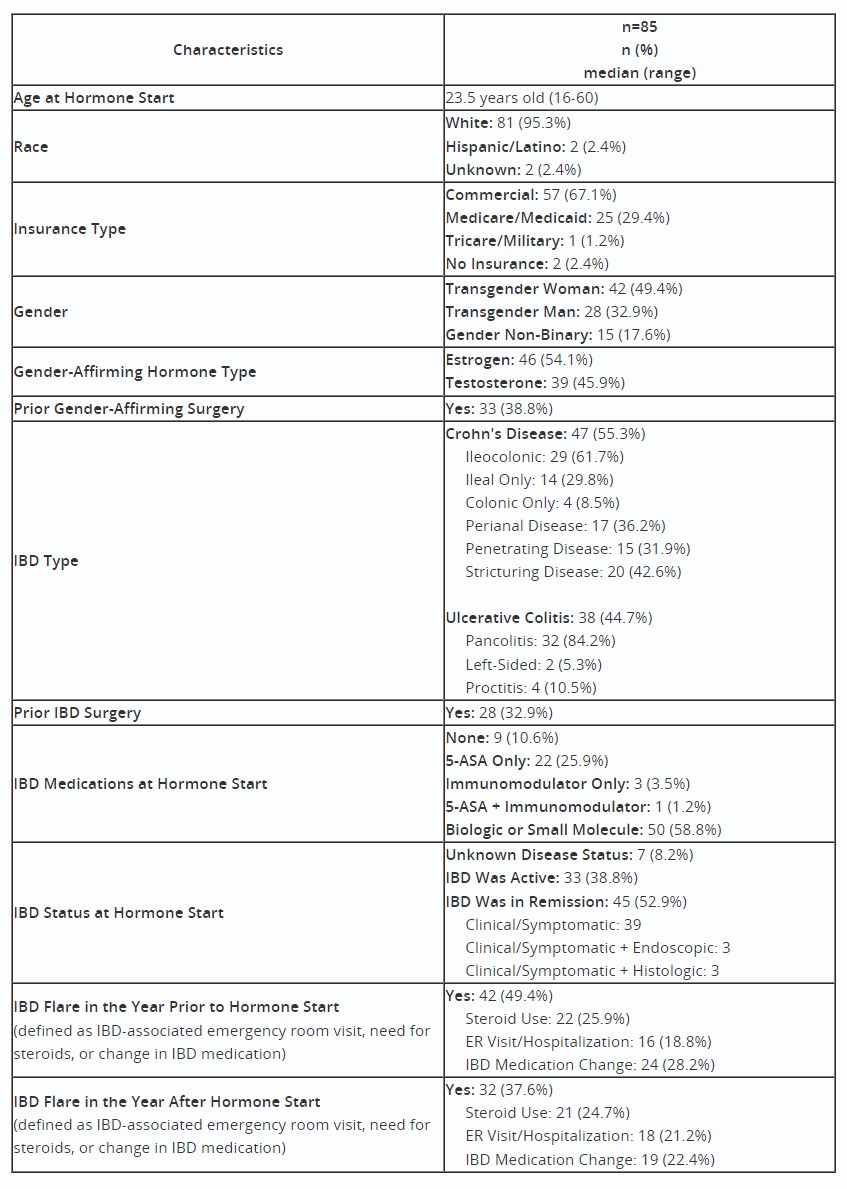
Table: Patient Characteristics and Details of IBD Flare
Disclosures:
Austin Lin indicated no relevant financial relationships.
Jenna Davison indicated no relevant financial relationships.
Shravya Pothula indicated no relevant financial relationships.
Justin Field indicated no relevant financial relationships.
Kira Newman: Pfizer – Grant/Research Support.
Sara Horst: AbbVie – Consultant. Bristol Myers Squibb – Consultant. Janssen – Consultant. Pfizer – Consultant. Takeda – Consultant.
Benjamin Click: AbbVie – Consultant. BMS – Consultant. Janssen – Consultant. Pfizer – Consultant. Prometheus – Consultant. Takeda – Consultant. TARGET-RWE – Consultant.
Victor Chedid indicated no relevant financial relationships.
Audrey Bennett: Celltrion – Consultant.
Austin Lin, MD1, Jenna Davison, MD, MPH2, Shravya Pothula, MD3, Justin Field, MD4, Kira L. Newman, MD, PhD1, Sara N. Horst, MD5, Benjamin Click, MD3, Victor Chedid, MD, MS2, Audrey Bennett, MD6, 67, Impact of Gender-Affirming Hormone Therapy in Transgender and Gender Non-Conforming Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.



