Oral Paper Presentation
Annual Scientific Meeting
Session: Presidential Plenary Session 1
1 - Artificial Intelligence-Driven Endoscopic Ultrasound for Detection and Differentiation of Pleomorphic Pancreatic Lesions: A Transatlantic Study
Monday, October 28, 2024
8:00 AM - 8:12 AM ET
Location: Terrace Ballroom

Miguel Mascarenhas, MD, PhD
Centro Hospitalar Universitário de São João
Porto, Porto, Portugal
Presenting Author(s)
Award: ACG International Award
Francisco Mendes, MD1, Miguel Mascarenhas, MD, PhD1, Jessica Widmer, MD2, Mariano González-Haba, MD3, Tamas Gonda, MD4, Belen Agudo, MD3, Tiago Ribeiro, MD1, Miguel Martins, MD1, Maria joão Almeida, MD5, Antonio Pinto da Costa, MD6, Yousef Fazel, MD2, Marcos Eduardo Lera dos Santos, MD, PhD7, Eduardo Horneaux de Moura, MD, PhD7, Alexandre Bestetti, MD7, Filipe Vilas Boas, MD, PhD5, Pedro Moutinho Ribeiro, MD, PhD5, Susana Lopes, MD, PhD, FACG1, Joana Fernandes, BSc8, João Ferreira, PhD8, Guilherme Macedo, MD, PhD, FACG1
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2NYU Langone Health, New York, NY; 3Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Madrid, Spain; 4New York University Langone Health, New York, NY; 5Centro Hospitalar Universitário São João, Porto, Porto, Portugal; 6Hospital Universitario Puerta de Hierro-Majadahonda, Madrid, Madrid, Spain; 7Hospital das Clínicas da Faculdade de Medicina da Universidade de Sao Paulo, São Paulo, Sao Paulo, Brazil; 8Faculdade de Engenharia da Universidade do Porto, Porto, Porto, Portugal
Introduction: Endoscopic ultrasound (EUS) allows characterization and tissue sampling of pancreatic lesions. Pancreatic cystic neoplasms (PCN) include mucinous (M-PCN) and non-mucinous lesions (NM-PCN). Pancreatic adenocarcinoma (P-ADC) is the commonest pancreatic solid lesion (PSL), followed by pancreatic neuroendocrine tumor (P-NET). While EUS is preferred for pancreatic lesion evaluation, its diagnostic accuracy is suboptimal. This multicentric study aims to develop a convolutional neural network (CNN) for detecting and distinguishing cystic (namely M-PCN and NM-PCN) and solid (particularly P-ADC and P-NET) pancreatic lesions.
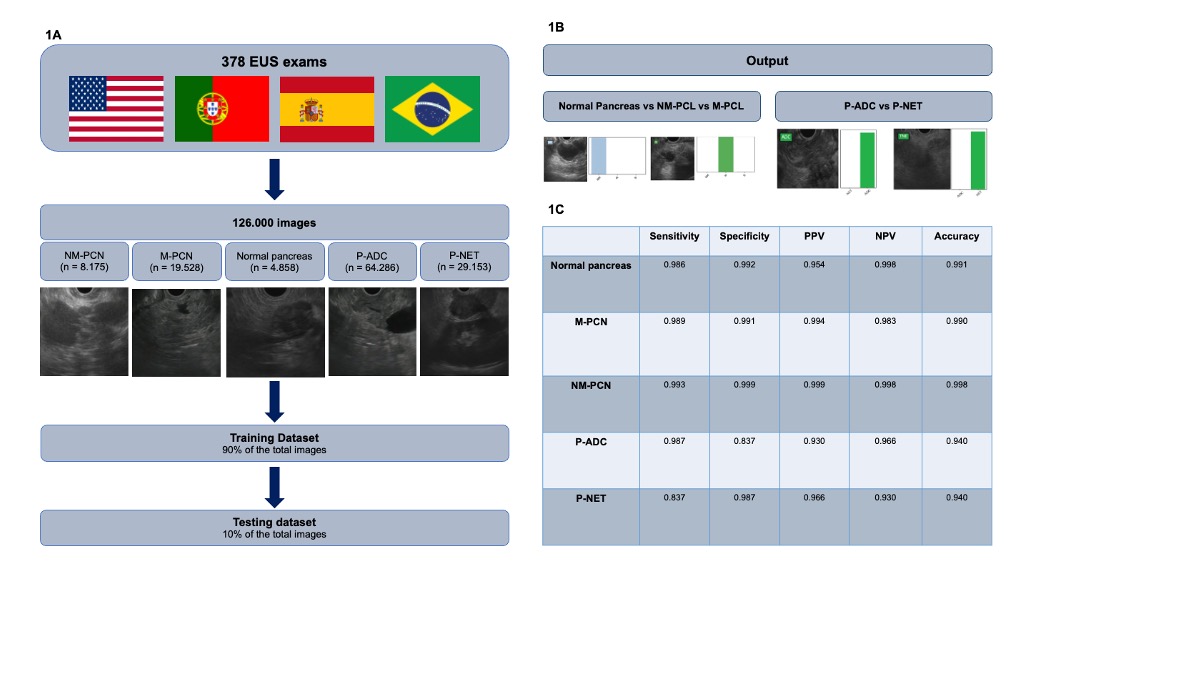
Methods: A CNN was developed with 378 EUS exams from 4 international reference centers from Portugal, Spain, the United States of America and Brazil. 126.000 images were obtained – 19.528 M-PCN, 8.175 NM-PCN, 64.286 P-ADC, 29.153 P-NET and 4.858 normal pancreas images. A trinary CNN differentiated normal pancreas tissue from mucinous and non-mucinous pancreatic cystic lesions. A binary CNN distinguished P-ADC from P-NET. The total dataset was divided in a training and testing dataset (used for model’s evaluation) in a 90/10% ratio. The model was evaluated through its sensitivity, specificity, positive and negative predictive values and accuracy.
Results: The CNN had 99.1% accuracy for identifying normal pancreatic tissue, with 99.0% and 99.8% accuracy for M-PCN and NM-PCN, respectively. P-ADC and P-NET were distinguished with 94.0% accuracy, with 98.7% and 83.7% sensitivities for P-ADC and P-NET, respectively.
Discussion: Our group developed the first worldwide CNN capable of detecting and differentiating the commonest cystic and solid pancreatic lesions in EUS images. The model results were based on a large dataset from 4 centers in two continents, minimizing the impact of the demographic bias. The development of artificial intelligence models is of uttermost importance for augmenting EUS diagnostic accuracy, and the availableness of a technology that is efficient in detecting both PCN (differencing them from normal pancreatic tissue) and PSL is a proof of methodological development and robustness. Larger real-time multicentric studies are needed for technology implementation.
Disclosures:
Francisco Mendes, MD1, Miguel Mascarenhas, MD, PhD1, Jessica Widmer, MD2, Mariano González-Haba, MD3, Tamas Gonda, MD4, Belen Agudo, MD3, Tiago Ribeiro, MD1, Miguel Martins, MD1, Maria joão Almeida, MD5, Antonio Pinto da Costa, MD6, Yousef Fazel, MD2, Marcos Eduardo Lera dos Santos, MD, PhD7, Eduardo Horneaux de Moura, MD, PhD7, Alexandre Bestetti, MD7, Filipe Vilas Boas, MD, PhD5, Pedro Moutinho Ribeiro, MD, PhD5, Susana Lopes, MD, PhD, FACG1, Joana Fernandes, BSc8, João Ferreira, PhD8, Guilherme Macedo, MD, PhD, FACG1, 1, Artificial Intelligence-Driven Endoscopic Ultrasound for Detection and Differentiation of Pleomorphic Pancreatic Lesions: A Transatlantic Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Francisco Mendes, MD1, Miguel Mascarenhas, MD, PhD1, Jessica Widmer, MD2, Mariano González-Haba, MD3, Tamas Gonda, MD4, Belen Agudo, MD3, Tiago Ribeiro, MD1, Miguel Martins, MD1, Maria joão Almeida, MD5, Antonio Pinto da Costa, MD6, Yousef Fazel, MD2, Marcos Eduardo Lera dos Santos, MD, PhD7, Eduardo Horneaux de Moura, MD, PhD7, Alexandre Bestetti, MD7, Filipe Vilas Boas, MD, PhD5, Pedro Moutinho Ribeiro, MD, PhD5, Susana Lopes, MD, PhD, FACG1, Joana Fernandes, BSc8, João Ferreira, PhD8, Guilherme Macedo, MD, PhD, FACG1
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2NYU Langone Health, New York, NY; 3Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Madrid, Spain; 4New York University Langone Health, New York, NY; 5Centro Hospitalar Universitário São João, Porto, Porto, Portugal; 6Hospital Universitario Puerta de Hierro-Majadahonda, Madrid, Madrid, Spain; 7Hospital das Clínicas da Faculdade de Medicina da Universidade de Sao Paulo, São Paulo, Sao Paulo, Brazil; 8Faculdade de Engenharia da Universidade do Porto, Porto, Porto, Portugal
Introduction: Endoscopic ultrasound (EUS) allows characterization and tissue sampling of pancreatic lesions. Pancreatic cystic neoplasms (PCN) include mucinous (M-PCN) and non-mucinous lesions (NM-PCN). Pancreatic adenocarcinoma (P-ADC) is the commonest pancreatic solid lesion (PSL), followed by pancreatic neuroendocrine tumor (P-NET). While EUS is preferred for pancreatic lesion evaluation, its diagnostic accuracy is suboptimal. This multicentric study aims to develop a convolutional neural network (CNN) for detecting and distinguishing cystic (namely M-PCN and NM-PCN) and solid (particularly P-ADC and P-NET) pancreatic lesions.
Methods: A CNN was developed with 378 EUS exams from 4 international reference centers from Portugal, Spain, the United States of America and Brazil. 126.000 images were obtained – 19.528 M-PCN, 8.175 NM-PCN, 64.286 P-ADC, 29.153 P-NET and 4.858 normal pancreas images. A trinary CNN differentiated normal pancreas tissue from mucinous and non-mucinous pancreatic cystic lesions. A binary CNN distinguished P-ADC from P-NET. The total dataset was divided in a training and testing dataset (used for model’s evaluation) in a 90/10% ratio. The model was evaluated through its sensitivity, specificity, positive and negative predictive values and accuracy.
Results: The CNN had 99.1% accuracy for identifying normal pancreatic tissue, with 99.0% and 99.8% accuracy for M-PCN and NM-PCN, respectively. P-ADC and P-NET were distinguished with 94.0% accuracy, with 98.7% and 83.7% sensitivities for P-ADC and P-NET, respectively.
Discussion: Our group developed the first worldwide CNN capable of detecting and differentiating the commonest cystic and solid pancreatic lesions in EUS images. The model results were based on a large dataset from 4 centers in two continents, minimizing the impact of the demographic bias. The development of artificial intelligence models is of uttermost importance for augmenting EUS diagnostic accuracy, and the availableness of a technology that is efficient in detecting both PCN (differencing them from normal pancreatic tissue) and PSL is a proof of methodological development and robustness. Larger real-time multicentric studies are needed for technology implementation.
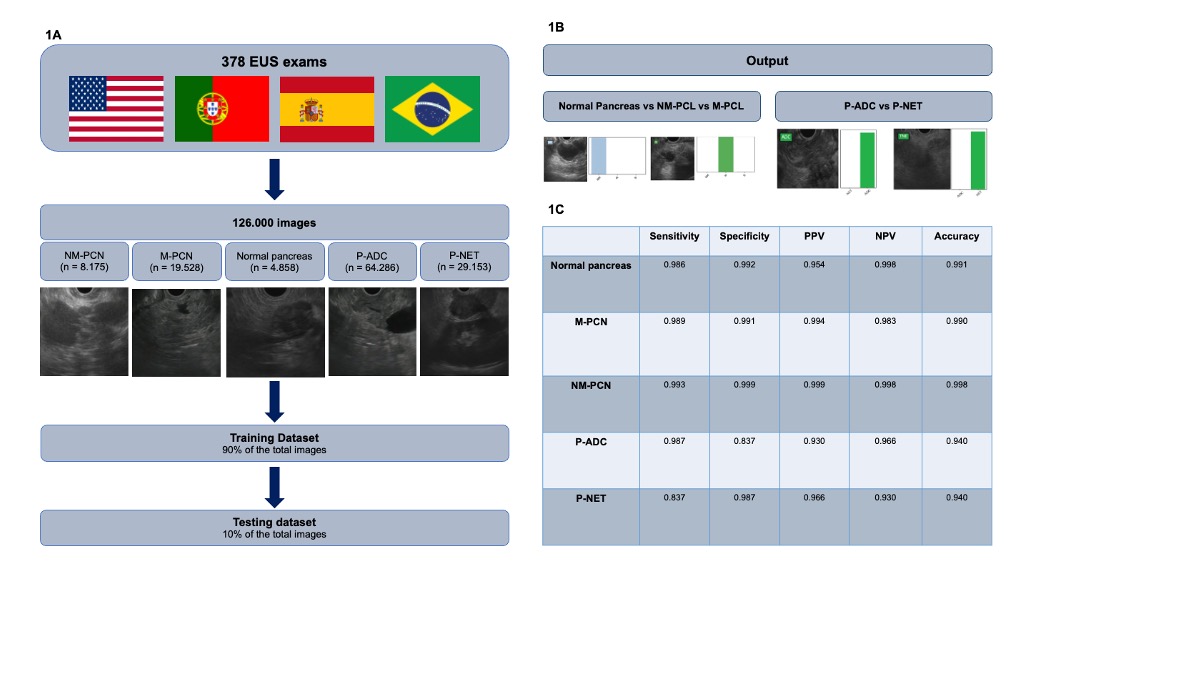
Figure: Figure 1 – Artificial intelligence-driven endoscopic ultrasound for detection and differentiation of pleomorphic pancreatic lesions: a Transatlantic Study 1A - Study design for the development of the convolutional neural network. 1B – Output obtained from the convolutional neural network. The bars are a representation of the estimated probability by the CNN. 1C - Performance measures of the testing dataset for detection and differentiation of normal pancreas images, pancreatic cystic lesions and pancreatic solid lesions. NM-PCL – non mucinous pancreatic cystic neoplasm; M-PCL – mucinous pancreatic cystic neoplasm; P-ADC – pancreatic adenocarcinoma; P-NET – pancreatic neuroendocrine tumor; NM – non mucinous; M – mucinous; N – normal; ADC – adenocarcinoma; NET – neuroendocrine tumor. Sn – sensitivity; Sp – specificity; PPV – positive predictive value; NPV – negative predictive value; Acc – accuracy.
Disclosures:
Francisco Mendes indicated no relevant financial relationships.
Miguel Mascarenhas indicated no relevant financial relationships.
Jessica Widmer indicated no relevant financial relationships.
Mariano González-Haba indicated no relevant financial relationships.
Tamas Gonda indicated no relevant financial relationships.
Belen Agudo indicated no relevant financial relationships.
Tiago Ribeiro indicated no relevant financial relationships.
Miguel Martins indicated no relevant financial relationships.
Maria joão Almeida indicated no relevant financial relationships.
Antonio Pinto da Costa indicated no relevant financial relationships.
Yousef Fazel indicated no relevant financial relationships.
Marcos Eduardo Lera dos Santos indicated no relevant financial relationships.
Eduardo Horneaux de Moura indicated no relevant financial relationships.
Alexandre Bestetti indicated no relevant financial relationships.
Filipe Vilas Boas indicated no relevant financial relationships.
Pedro Moutinho Ribeiro indicated no relevant financial relationships.
Susana Lopes indicated no relevant financial relationships.
Joana Fernandes indicated no relevant financial relationships.
João Ferreira indicated no relevant financial relationships.
Guilherme Macedo indicated no relevant financial relationships.
Francisco Mendes, MD1, Miguel Mascarenhas, MD, PhD1, Jessica Widmer, MD2, Mariano González-Haba, MD3, Tamas Gonda, MD4, Belen Agudo, MD3, Tiago Ribeiro, MD1, Miguel Martins, MD1, Maria joão Almeida, MD5, Antonio Pinto da Costa, MD6, Yousef Fazel, MD2, Marcos Eduardo Lera dos Santos, MD, PhD7, Eduardo Horneaux de Moura, MD, PhD7, Alexandre Bestetti, MD7, Filipe Vilas Boas, MD, PhD5, Pedro Moutinho Ribeiro, MD, PhD5, Susana Lopes, MD, PhD, FACG1, Joana Fernandes, BSc8, João Ferreira, PhD8, Guilherme Macedo, MD, PhD, FACG1, 1, Artificial Intelligence-Driven Endoscopic Ultrasound for Detection and Differentiation of Pleomorphic Pancreatic Lesions: A Transatlantic Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.



