Oral Paper Presentation
Annual Scientific Meeting
Session: Presidential Plenary Session 2
8 - Primary Sclerosing Cholangitis in the Absence of Inflammatory Bowel Disease Increases the Risk of Colorectal Cancer: A Propensity-Matched Cohort Study
Monday, October 28, 2024
9:54 AM - 10:06 AM ET
Location: Terrace Ballroom
.jpg)
Saqr Alsakarneh, MD (he/him/his)
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Saqr Alsakarneh, MD1, Fouad Jaber, MD1, Adam S.. Faye, MD2, Jana G. Hashash, MD, MSc3, Mohammad Bilal, MD4, Aasma Shaukat, MD, MPH5
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2NYU Grossman School of Medicine, New York, NY; 3Mayo Clinic, Jacksonville, FL; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 5NYU Langone Health, New York, NY
Introduction: Patients with primary sclerosing cholangitis (PSC) and concomitant inflammatory bowel disease (IBD) are at increased risk of colorectal cancer (CRC). However, the risk of CRC in patients with PSC without IBD remains uncertain. We aimed to evaluate the risk of CRC in patients with PSC without a history of IBD using a large national database.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify patients ≥18 years with PSC. Patients were then divided into 2 groups, PSC with IBD (PSC-IBD cohort) and PSC without IBD (PSC non-IBD cohort), and were matched with patients without a history of PSC or IBD (non-PSC/non-IBD group) by using 1:1 propensity score matching (Table 1). The primary outcome was the risk of first diagnosis of CRC that occurred within 14 years from the index event (diagnosis of PSC). Secondary outcomes included a comparison of CRC risk in PSC with IBD with subgroup analyses for UC and CD, risk of other gastrointestinal malignancies, and CRC risk stratified by age and gender. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs were used to compare time-to-event rates at daily time intervals.
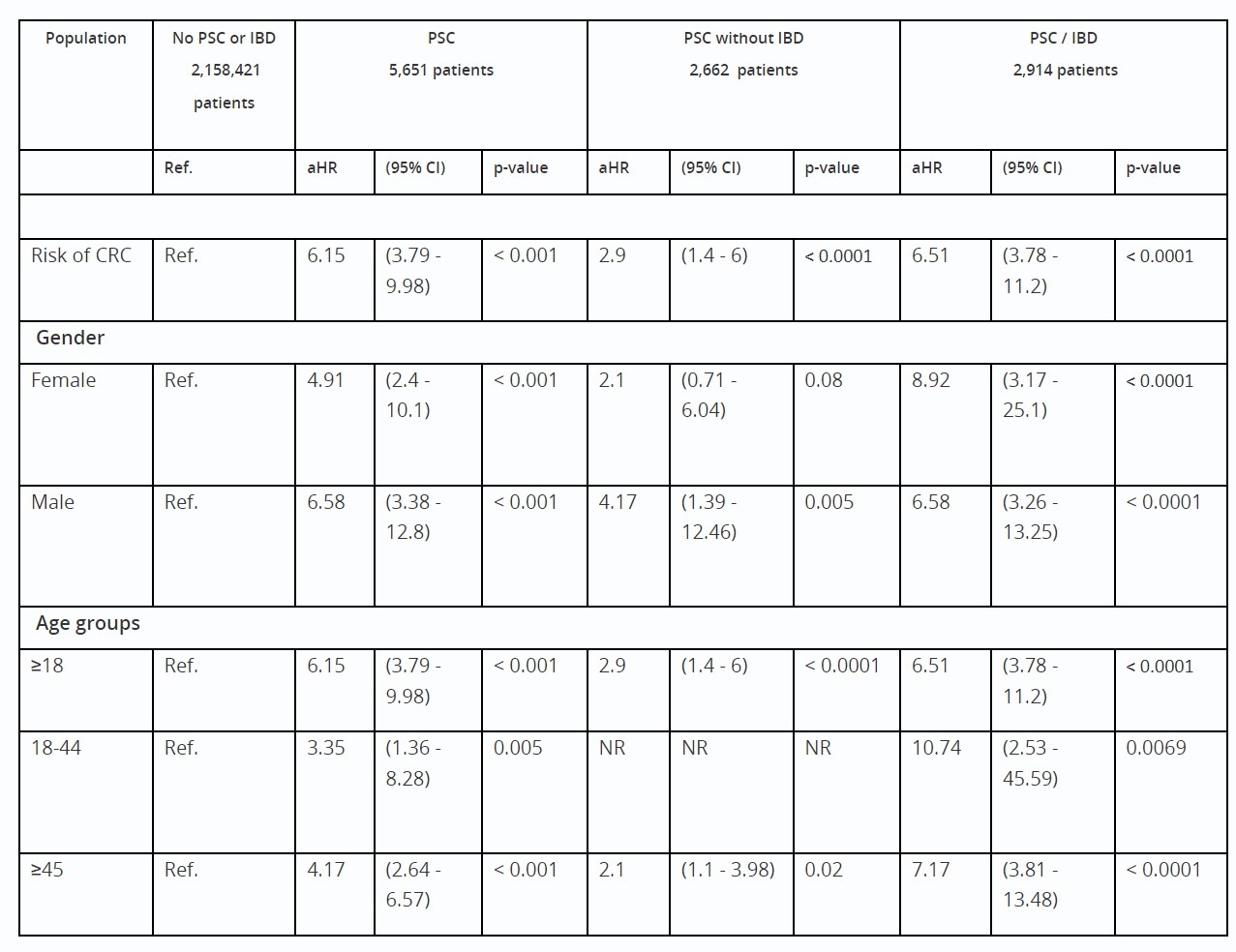
Results: Among 2,662 patients with PSC but no IBD, the mean age was 51.6 ± 18.1 years, and 47.2% were females. PSC patients without IBD were at increased risk of CRC compared to the non-PSC/IBD cohort (aHR = 2.9; 95% CI: 1.6 – 6.0). While males (aHR = 4.17; 95% CI: 1.4 – 12.5) had an increased risk of CRC, females (aHR = 2.1; 95% CI: 0.8 – 6.1) did not show an increased risk compared to the general population (Table 1).
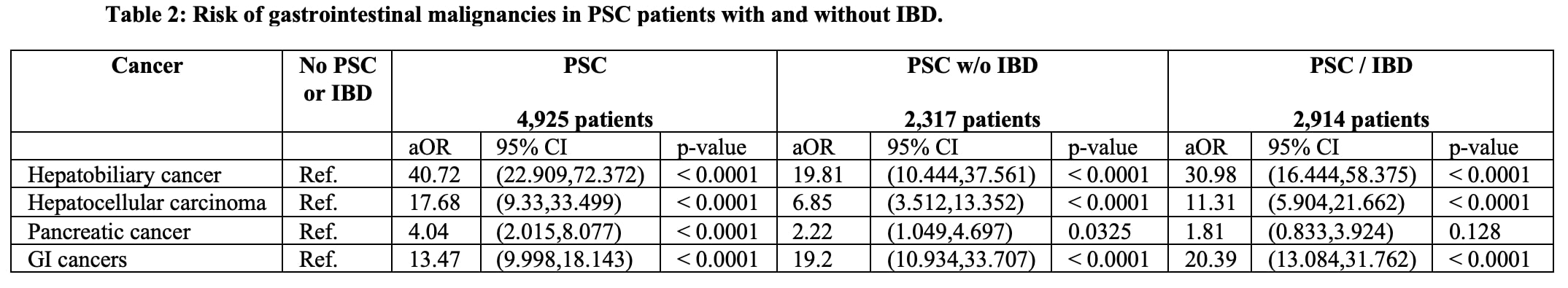
Patients with PSC and IBD exhibited a higher risk of CRC (aHR = 6.5; 95% CI: 3.78 - 11.2), especially among the UC cohort (aHR = 6.3; 95% CI: 3.2 - 12.4). Consistent findings were observed in women, men, and different age groups (Table 1). Patients with PSC were at increased risk of various gastrointestinal malignancies (aHR = 10.5; 95% CI: 7.3 - 15; P < .0001), including hepatobiliary cancers, pancreatic cancer, and hepatocellular carcinoma (Table 2).
Discussion: Our results provide real-world evidence that PSC is an independent risk factor for CRC development, even among those without concomitant IBD. These findings suggest that current guidelines should incorporate the presence of PSC, independent of IBD, into the current screening guidelines for CRC.
Disclosures:
Saqr Alsakarneh, MD1, Fouad Jaber, MD1, Adam S.. Faye, MD2, Jana G. Hashash, MD, MSc3, Mohammad Bilal, MD4, Aasma Shaukat, MD, MPH5, 8, Primary Sclerosing Cholangitis in the Absence of Inflammatory Bowel Disease Increases the Risk of Colorectal Cancer: A Propensity-Matched Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2NYU Grossman School of Medicine, New York, NY; 3Mayo Clinic, Jacksonville, FL; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 5NYU Langone Health, New York, NY
Introduction: Patients with primary sclerosing cholangitis (PSC) and concomitant inflammatory bowel disease (IBD) are at increased risk of colorectal cancer (CRC). However, the risk of CRC in patients with PSC without IBD remains uncertain. We aimed to evaluate the risk of CRC in patients with PSC without a history of IBD using a large national database.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify patients ≥18 years with PSC. Patients were then divided into 2 groups, PSC with IBD (PSC-IBD cohort) and PSC without IBD (PSC non-IBD cohort), and were matched with patients without a history of PSC or IBD (non-PSC/non-IBD group) by using 1:1 propensity score matching (Table 1). The primary outcome was the risk of first diagnosis of CRC that occurred within 14 years from the index event (diagnosis of PSC). Secondary outcomes included a comparison of CRC risk in PSC with IBD with subgroup analyses for UC and CD, risk of other gastrointestinal malignancies, and CRC risk stratified by age and gender. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs were used to compare time-to-event rates at daily time intervals.
Results: Among 2,662 patients with PSC but no IBD, the mean age was 51.6 ± 18.1 years, and 47.2% were females. PSC patients without IBD were at increased risk of CRC compared to the non-PSC/IBD cohort (aHR = 2.9; 95% CI: 1.6 – 6.0). While males (aHR = 4.17; 95% CI: 1.4 – 12.5) had an increased risk of CRC, females (aHR = 2.1; 95% CI: 0.8 – 6.1) did not show an increased risk compared to the general population (Table 1).
Patients with PSC and IBD exhibited a higher risk of CRC (aHR = 6.5; 95% CI: 3.78 - 11.2), especially among the UC cohort (aHR = 6.3; 95% CI: 3.2 - 12.4). Consistent findings were observed in women, men, and different age groups (Table 1). Patients with PSC were at increased risk of various gastrointestinal malignancies (aHR = 10.5; 95% CI: 7.3 - 15; P < .0001), including hepatobiliary cancers, pancreatic cancer, and hepatocellular carcinoma (Table 2).
Discussion: Our results provide real-world evidence that PSC is an independent risk factor for CRC development, even among those without concomitant IBD. These findings suggest that current guidelines should incorporate the presence of PSC, independent of IBD, into the current screening guidelines for CRC.
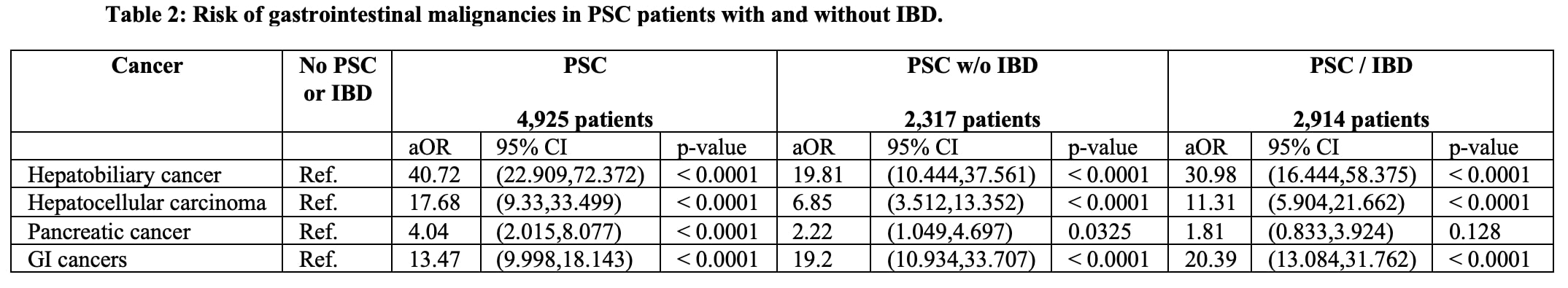
Figure: Table 2: Risk of gastrointestinal malignancies in primary sclerosing cholangitis patients with and without concomitant inflammatory bowel disease.
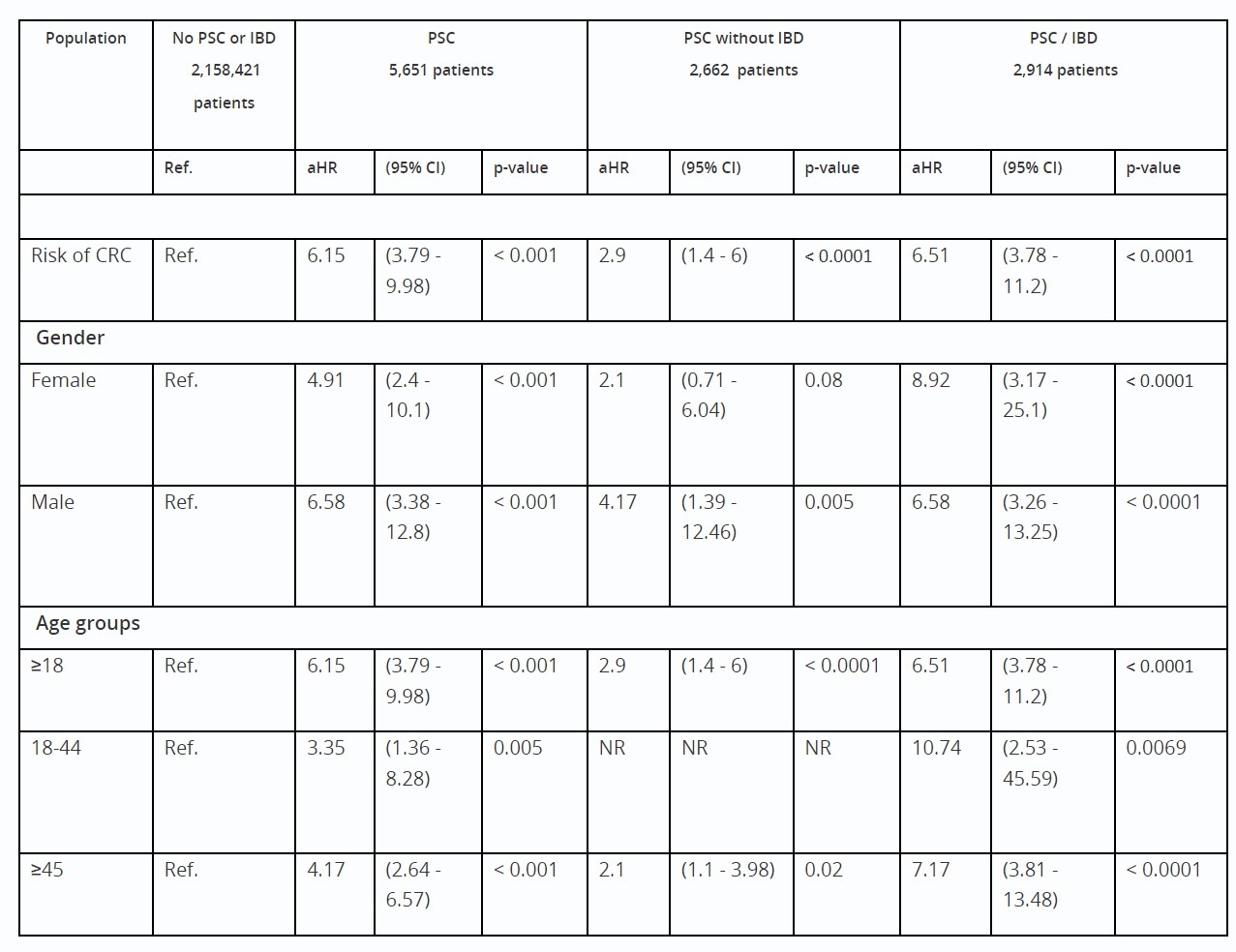
Table: Table 1: Risk of colorectal cancer in patients with primary sclerosing cholangitis with and without concomitant inflammatory bowel disease.
Abbreviations: aHR: Adjusted hazardous ratio; PSC: Primary sclerosing cholangitis; IBD: Inflammatory bowel disease; ref: reference group; NR: Not reported
* Cohorts were propensity score matched (1:1) for demographics (age, sex, race, and ethnicity), adverse socioeconomic determinants of health, preexisting medical conditions, family and personal history of cancers and colonic polyps, lifestyle factors (exercise, diet, smoking, and alcohol drinking), procedures such as colonoscopy and radiation therapy, aspirin, non-steroidal anti-inflammatory drugs, and IBD medications
Abbreviations: aHR: Adjusted hazardous ratio; PSC: Primary sclerosing cholangitis; IBD: Inflammatory bowel disease; ref: reference group; NR: Not reported
* Cohorts were propensity score matched (1:1) for demographics (age, sex, race, and ethnicity), adverse socioeconomic determinants of health, preexisting medical conditions, family and personal history of cancers and colonic polyps, lifestyle factors (exercise, diet, smoking, and alcohol drinking), procedures such as colonoscopy and radiation therapy, aspirin, non-steroidal anti-inflammatory drugs, and IBD medications
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Fouad Jaber indicated no relevant financial relationships.
Adam Faye: Abbvie – Consultant. BMS – Consultant. Takeda – Education Seminar.
Jana Hashash: Bristol Myers Squibb – Consultant.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Aasma Shaukat: iterative health; Freenome – Consultant.
Saqr Alsakarneh, MD1, Fouad Jaber, MD1, Adam S.. Faye, MD2, Jana G. Hashash, MD, MSc3, Mohammad Bilal, MD4, Aasma Shaukat, MD, MPH5, 8, Primary Sclerosing Cholangitis in the Absence of Inflammatory Bowel Disease Increases the Risk of Colorectal Cancer: A Propensity-Matched Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


