Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 1B: Interventional Endoscopy
17 - Postoperative Abdominal Fluid Collections Management with EUS-Guided Transmural Drainage: Timing, Efficacy, and Safety Profile
Monday, October 28, 2024
2:35 PM - 2:45 PM ET
Location: Terrace Ballroom 2-3

Muhammad H. Raza, MD (he/him/his)
New York-Presbyterian/Columbia University Irving Medical Center
New York, NY
Presenting Author(s)
Muhammad H. Raza, MD1, Jonathan R. Tiao, MD1, Lyndon Luk, MD1, John B. Doyle, MD1, Kazuki N. Sugahara, MD, PhD2, Beth A. Schrope, MD, PhD1, Michael D. Kluger, MD, MPH1, John A. Chabot, MD1, Tamas A.. Gonda, MD3, John M. Poneros, MD1, Amrita Sethi, MD1, Kavel H. Visrodia, MD1
1New York-Presbyterian/Columbia University Irving Medical Center, New York, NY; 2Columbia University Irving Medical Center, New York, NY; 3NYU Grossman School of Medicine, New York, NY
Introduction: Symptomatic postoperative fluid collections (POFCs) can result in morbidity and mortality after abdominal surgery requiring timely intervention. EUS-guided drainage has traditionally been postponed up to 4 weeks postoperatively to ensure a mature wall has completely formed, thereby reducing the risks of perforation or peritonitis. However, some POFCs may be amenable to intervention sooner. The purpose of this study was to compare the efficacy and safety profile of acute (≤15 days), early (16-30 days), and delayed ( >30 days) EUS-guided drainage of POFCs.
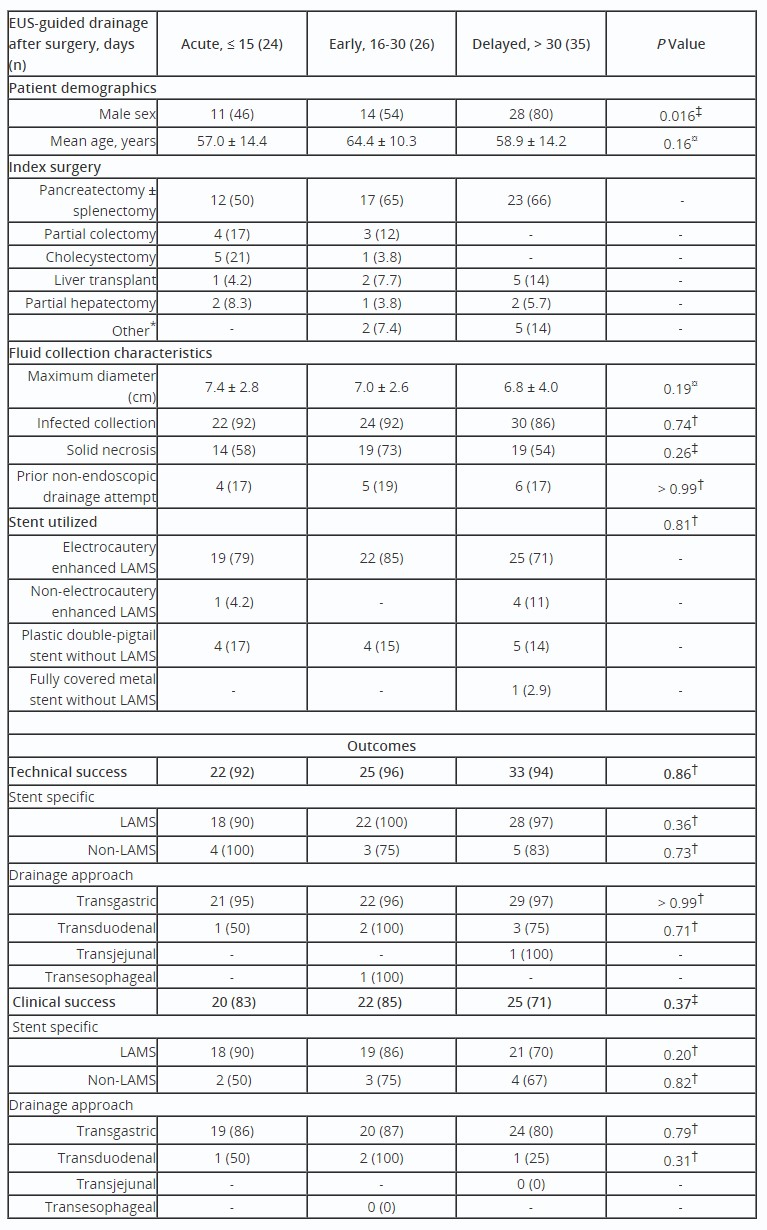
Methods: A retrospective cohort of patients with symptomatic POFCs after any abdominal surgery undergoing EUS-guided drainage from 2013 to 2023 after multidisciplinary discussion at a single tertiary care center were identified. Patient characteristics, procedural data, and outcomes were examined. Technical success was defined as the ability to access and drain a POFC using transmural stents on initial endoscopy. Clinical success was defined as radiographically or endosonographically confirmed symptomatic improvement of the target POFC after EUS-guided drainage without need for further percutaneous or surgical intervention.
Results: Among 85 patients, 50 (59%) underwent EUS-guided drainage ≤30 days after surgery, with 48% (n=24) managed acutely. The index surgery in 61% of patients was distal pancreatectomy with splenectomy (44%, n=23 for pancreatic ductal adenocarcinoma). Most patients (n=71, 83%) received lumen-apposing metal stents. Overall technical and clinical success rates were 94% and 79%, respectively, after a mean of 2.2 endoscopies (range 1-5). Technical and clinical success rates did not differ between acute, early, and delayed EUS-guided drainage (92% vs 96% vs 94%, and 83% vs 85% vs 71%, P=0.86 and P=0.37, respectively). Adverse events were similar across groups (P=0.85). Transgastric access was associated with clinical success (P< 0.001) and fewer adverse events (P=0.03), while transduodenal access predicted technical (P=0.05) and clinical failure (P=0.02).
Discussion: In this large single-center experience of symptomatic POFCs, acute and early EUS-guided drainage with lumen-apposing metal stents in carefully selected patients was found to be technically safe and clinically effective, avoiding potentially more morbid interventions such as ERCP, percutaneous drainage, or surgery. Further randomized, prospective studies to investigate predictors of technical and clinical success as well as adverse events are warranted.
Disclosures:
Muhammad H. Raza, MD1, Jonathan R. Tiao, MD1, Lyndon Luk, MD1, John B. Doyle, MD1, Kazuki N. Sugahara, MD, PhD2, Beth A. Schrope, MD, PhD1, Michael D. Kluger, MD, MPH1, John A. Chabot, MD1, Tamas A.. Gonda, MD3, John M. Poneros, MD1, Amrita Sethi, MD1, Kavel H. Visrodia, MD1, 17, Postoperative Abdominal Fluid Collections Management with EUS-Guided Transmural Drainage: Timing, Efficacy, and Safety Profile, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian/Columbia University Irving Medical Center, New York, NY; 2Columbia University Irving Medical Center, New York, NY; 3NYU Grossman School of Medicine, New York, NY
Introduction: Symptomatic postoperative fluid collections (POFCs) can result in morbidity and mortality after abdominal surgery requiring timely intervention. EUS-guided drainage has traditionally been postponed up to 4 weeks postoperatively to ensure a mature wall has completely formed, thereby reducing the risks of perforation or peritonitis. However, some POFCs may be amenable to intervention sooner. The purpose of this study was to compare the efficacy and safety profile of acute (≤15 days), early (16-30 days), and delayed ( >30 days) EUS-guided drainage of POFCs.
Methods: A retrospective cohort of patients with symptomatic POFCs after any abdominal surgery undergoing EUS-guided drainage from 2013 to 2023 after multidisciplinary discussion at a single tertiary care center were identified. Patient characteristics, procedural data, and outcomes were examined. Technical success was defined as the ability to access and drain a POFC using transmural stents on initial endoscopy. Clinical success was defined as radiographically or endosonographically confirmed symptomatic improvement of the target POFC after EUS-guided drainage without need for further percutaneous or surgical intervention.
Results: Among 85 patients, 50 (59%) underwent EUS-guided drainage ≤30 days after surgery, with 48% (n=24) managed acutely. The index surgery in 61% of patients was distal pancreatectomy with splenectomy (44%, n=23 for pancreatic ductal adenocarcinoma). Most patients (n=71, 83%) received lumen-apposing metal stents. Overall technical and clinical success rates were 94% and 79%, respectively, after a mean of 2.2 endoscopies (range 1-5). Technical and clinical success rates did not differ between acute, early, and delayed EUS-guided drainage (92% vs 96% vs 94%, and 83% vs 85% vs 71%, P=0.86 and P=0.37, respectively). Adverse events were similar across groups (P=0.85). Transgastric access was associated with clinical success (P< 0.001) and fewer adverse events (P=0.03), while transduodenal access predicted technical (P=0.05) and clinical failure (P=0.02).
Discussion: In this large single-center experience of symptomatic POFCs, acute and early EUS-guided drainage with lumen-apposing metal stents in carefully selected patients was found to be technically safe and clinically effective, avoiding potentially more morbid interventions such as ERCP, percutaneous drainage, or surgery. Further randomized, prospective studies to investigate predictors of technical and clinical success as well as adverse events are warranted.
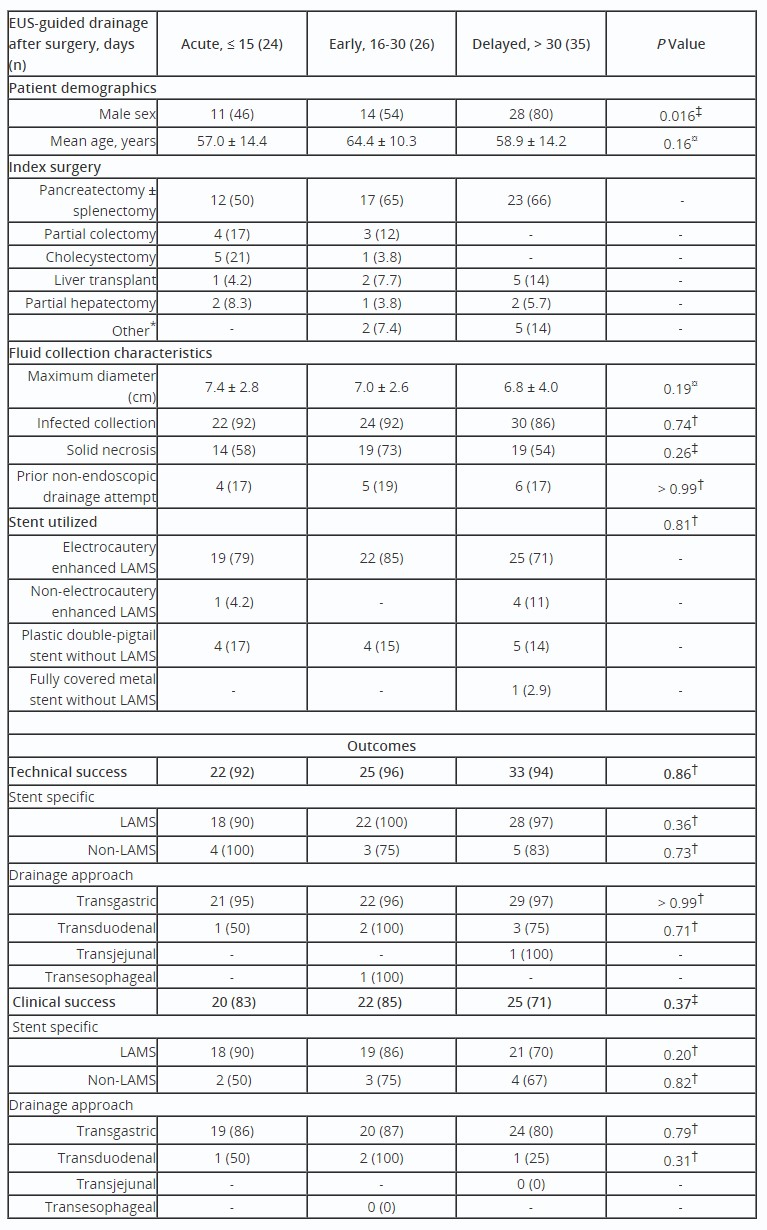
Table: Patient Characteristics, Fluid Collection Characteristics, and Outcomes Comparison of EUS-Guided Drainage. Values are n (%) unless otherwise defined.
¤ Kruskal-Wallis test; † Fisher’s exact test; ‡ Pearson’s Chi-squared test.
*Other surgeries (n = 7) included adrenalectomy (1), gastrojejunostomy with pyloroplasty (1), median arcuate ligament syndrome repair (1), partial gastrectomy with jejunostomy (1), proximal gastrectomy with splenectomy (1), sleeve gastrectomy (1), and deceased donor renal transplant (1).
¤ Kruskal-Wallis test; † Fisher’s exact test; ‡ Pearson’s Chi-squared test.
*Other surgeries (n = 7) included adrenalectomy (1), gastrojejunostomy with pyloroplasty (1), median arcuate ligament syndrome repair (1), partial gastrectomy with jejunostomy (1), proximal gastrectomy with splenectomy (1), sleeve gastrectomy (1), and deceased donor renal transplant (1).
Disclosures:
Muhammad Raza indicated no relevant financial relationships.
Jonathan Tiao indicated no relevant financial relationships.
Lyndon Luk indicated no relevant financial relationships.
John Doyle indicated no relevant financial relationships.
Kazuki Sugahara indicated no relevant financial relationships.
Beth Schrope indicated no relevant financial relationships.
Michael Kluger indicated no relevant financial relationships.
John Chabot indicated no relevant financial relationships.
Tamas Gonda indicated no relevant financial relationships.
John Poneros indicated no relevant financial relationships.
Amrita Sethi: Boston Scientific – Consultant, Grant/Research Support. Cook Medical – Consultant. Endosound – Advisor or Review Panel Member. ERBE – Grant/Research Support. Fujifilm – Grant/Research Support. Medtronic – Consultant. Olympus – Consultant. Pentax – Consultant.
Kavel Visrodia indicated no relevant financial relationships.
Muhammad H. Raza, MD1, Jonathan R. Tiao, MD1, Lyndon Luk, MD1, John B. Doyle, MD1, Kazuki N. Sugahara, MD, PhD2, Beth A. Schrope, MD, PhD1, Michael D. Kluger, MD, MPH1, John A. Chabot, MD1, Tamas A.. Gonda, MD3, John M. Poneros, MD1, Amrita Sethi, MD1, Kavel H. Visrodia, MD1, 17, Postoperative Abdominal Fluid Collections Management with EUS-Guided Transmural Drainage: Timing, Efficacy, and Safety Profile, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

