Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 1A: Colorectal Cancer Prevention
14 - Endoscopist Aggregated Hot Snare Polypectomy Rate Is Associated With Increased Risk of Colonoscopy Adverse Events
Monday, October 28, 2024
2:45 PM - 2:55 PM ET
Location: Terrace Ballroom 1

Seth Crockett, MD
Oregon Health & Science University
Portland, OR
Presenting Author(s)
Award: ACG Outstanding Research Award in the Colorectal Cancer Prevention Category
Seth Crockett, MD1, Jennifer Holub, MA, MPH2, Audrey H. Calderwood, MD, MS3, Rajesh N. Keswani, MD, MS4
1Oregon Health & Science University, Portland, OR; 2GI Quality Improvement Consortium, Ltd., Bethesda, MD; 3Dartmouth Hitchcock Medical Center, Lebanon, NH; 4Northwestern Feinberg School of Medicine, Chicago, IL
Introduction: In addition to polyp detection, polypectomy is a critical component of effective screening and surveillance colonoscopy. Polypectomy method impacts both the completeness of polypectomy and risk of adverse events. In particular, hot snare polypectomy is associated with a higher risk of post-polypectomy bleeding, yet hot snare use varies widely among endoscopists. We aimed to determine whether an aggregate measure of an endoscopist’s polypectomy practice (hot snare polypectomy rate: HSPR) was associated with colonoscopy adverse events.
Methods: We included complete screening and surveillance colonoscopies with one or more small ( < 1 cm) polyp(s) removed in patients aged 40-80 in the GIQuIC registry between 2019-2022. Diagnostic procedures, those with larger polyps or colorectal cancer, and inadequate bowel prep were excluded. Polypectomy technique was available through pre-set fields. The HSPR, defined as the proportion of colonoscopies with ≥1 small polyp during which HSP was used for at least one polyp, was calculated for each endoscopist. We then assessed whether patients had a 2nd colonoscopy within 30 days of the index exam for: A) any indication; or B) bleeding specifically. Bivariate proportions were compared by Chi-squared tests, and multivariable analysis was performed using logistic regression.
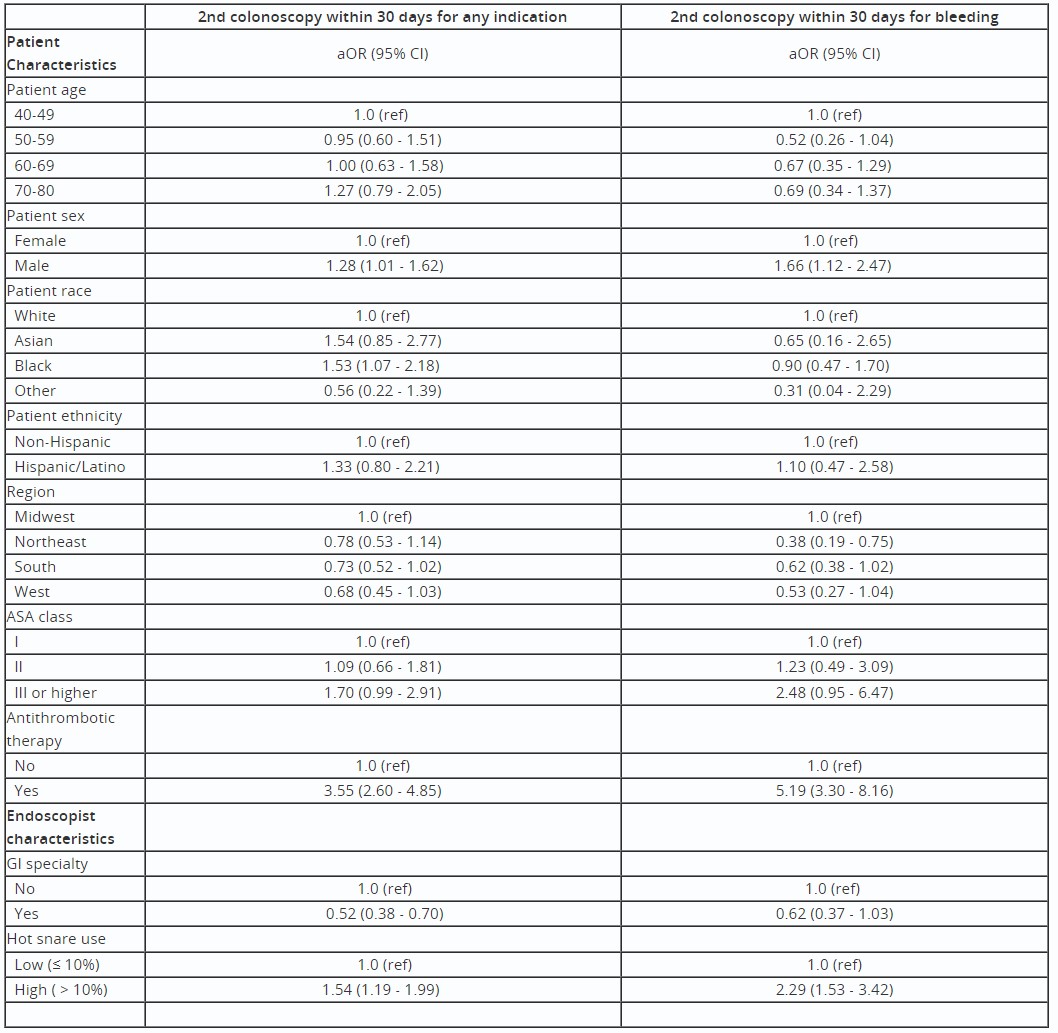
Results: We identified 1,572,414 unique patients who had ≥1 small polyp(s) removed. Among these, 291 patients had a 2nd colonoscopy within 30 days, 110 of which were for bleeding. Among the performing endoscopists (n=3,372), the mean HSPR (± SD) was 10.3% (±13.3). On multivariable analysis, controlling for potential patient-level confounders including age, sex, ASA classification, and antithrombotic use, GI specialty training was inversely associated with repeat colonoscopy (aOR 0.52, 95% CI 0.38, 0.70). In contrast, high endoscopist HSPR ( > 10%) was associated with increased risk of a 2nd colonoscopy both overall (aOR 1.54, 95% CI 1.19, 1.99) and for bleeding (aOR 2.29, 95% CI 1.53, 3.42) (Table).
Discussion: The risks of repeat colonoscopy and post-colonoscopy bleeding were higher for patients whose index colonoscopy was performed by endoscopists with high hot snare usage. Endoscopist-level training and quality improvement efforts directed at optimizing polypectomy practices may reduce the incidence of colonoscopy adverse events.
Disclosures:
Seth Crockett, MD1, Jennifer Holub, MA, MPH2, Audrey H. Calderwood, MD, MS3, Rajesh N. Keswani, MD, MS4, 14, Endoscopist Aggregated Hot Snare Polypectomy Rate Is Associated With Increased Risk of Colonoscopy Adverse Events, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Seth Crockett, MD1, Jennifer Holub, MA, MPH2, Audrey H. Calderwood, MD, MS3, Rajesh N. Keswani, MD, MS4
1Oregon Health & Science University, Portland, OR; 2GI Quality Improvement Consortium, Ltd., Bethesda, MD; 3Dartmouth Hitchcock Medical Center, Lebanon, NH; 4Northwestern Feinberg School of Medicine, Chicago, IL
Introduction: In addition to polyp detection, polypectomy is a critical component of effective screening and surveillance colonoscopy. Polypectomy method impacts both the completeness of polypectomy and risk of adverse events. In particular, hot snare polypectomy is associated with a higher risk of post-polypectomy bleeding, yet hot snare use varies widely among endoscopists. We aimed to determine whether an aggregate measure of an endoscopist’s polypectomy practice (hot snare polypectomy rate: HSPR) was associated with colonoscopy adverse events.
Methods: We included complete screening and surveillance colonoscopies with one or more small ( < 1 cm) polyp(s) removed in patients aged 40-80 in the GIQuIC registry between 2019-2022. Diagnostic procedures, those with larger polyps or colorectal cancer, and inadequate bowel prep were excluded. Polypectomy technique was available through pre-set fields. The HSPR, defined as the proportion of colonoscopies with ≥1 small polyp during which HSP was used for at least one polyp, was calculated for each endoscopist. We then assessed whether patients had a 2nd colonoscopy within 30 days of the index exam for: A) any indication; or B) bleeding specifically. Bivariate proportions were compared by Chi-squared tests, and multivariable analysis was performed using logistic regression.
Results: We identified 1,572,414 unique patients who had ≥1 small polyp(s) removed. Among these, 291 patients had a 2nd colonoscopy within 30 days, 110 of which were for bleeding. Among the performing endoscopists (n=3,372), the mean HSPR (± SD) was 10.3% (±13.3). On multivariable analysis, controlling for potential patient-level confounders including age, sex, ASA classification, and antithrombotic use, GI specialty training was inversely associated with repeat colonoscopy (aOR 0.52, 95% CI 0.38, 0.70). In contrast, high endoscopist HSPR ( > 10%) was associated with increased risk of a 2nd colonoscopy both overall (aOR 1.54, 95% CI 1.19, 1.99) and for bleeding (aOR 2.29, 95% CI 1.53, 3.42) (Table).
Discussion: The risks of repeat colonoscopy and post-colonoscopy bleeding were higher for patients whose index colonoscopy was performed by endoscopists with high hot snare usage. Endoscopist-level training and quality improvement efforts directed at optimizing polypectomy practices may reduce the incidence of colonoscopy adverse events.
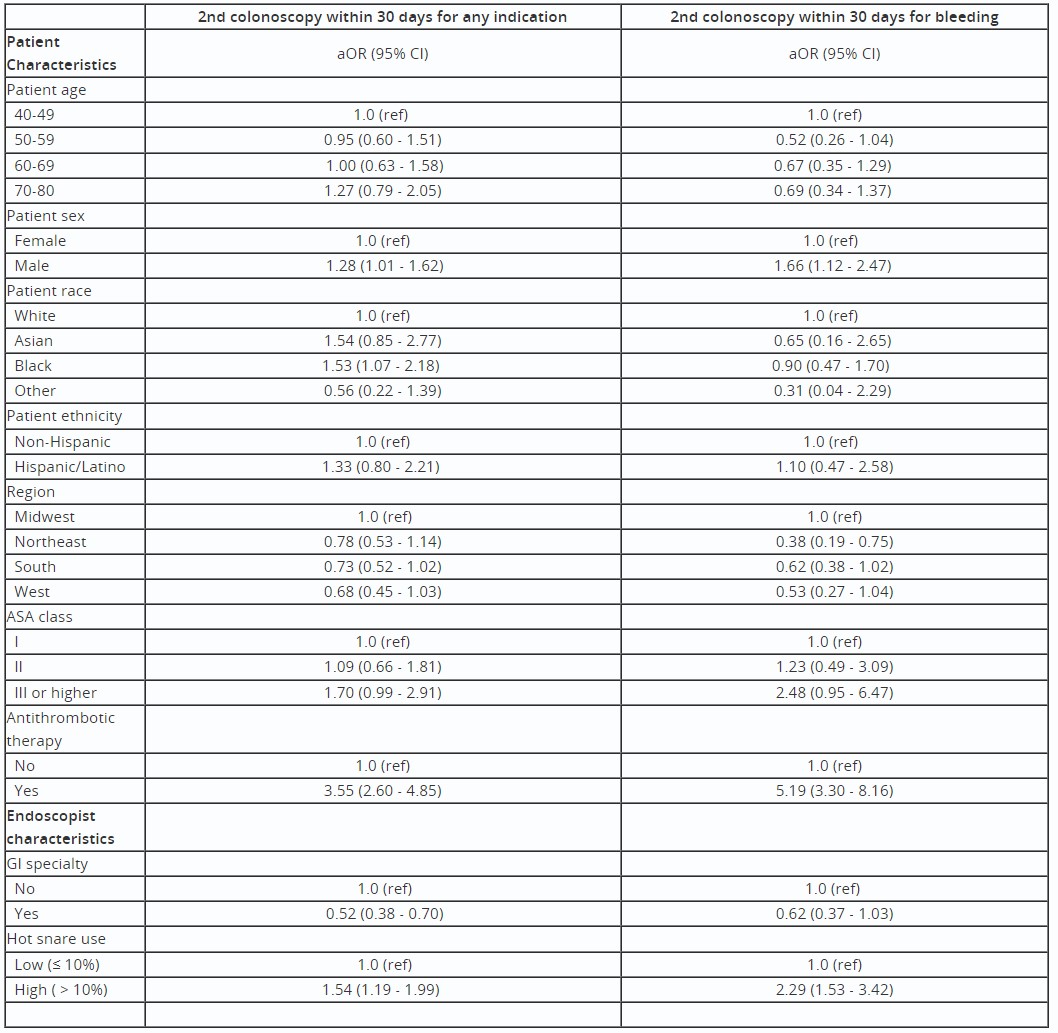
Table: Table: Multivariable analysis of patient and endoscopist factors associated with follow up colonoscopy, GIQuIC 2019-2022
Disclosures:
Seth Crockett indicated no relevant financial relationships.
Jennifer Holub indicated no relevant financial relationships.
Audrey Calderwood indicated no relevant financial relationships.
Rajesh Keswani indicated no relevant financial relationships.
Seth Crockett, MD1, Jennifer Holub, MA, MPH2, Audrey H. Calderwood, MD, MS3, Rajesh N. Keswani, MD, MS4, 14, Endoscopist Aggregated Hot Snare Polypectomy Rate Is Associated With Increased Risk of Colonoscopy Adverse Events, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

