Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 1B: Interventional Endoscopy
18 - A Quality Improvement Project: The ERAS Protocol Reduces Post Endoscopic Bariatric Procedure Healthcare Utilization
Monday, October 28, 2024
2:45 PM - 2:55 PM ET
Location: Terrace Ballroom 2-3

Farah Abdul Razzak, MD (she/her/hers)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Farah Abdul Razzak, MD1, Khushboo Gala, MBBS2, Karim Al Annan, MD3, Razan Aburumman, MD1, Anthony Kerbage, MD1, Rudy Mrad, MD1, Donna Maria Abboud, MD4, Barham Abu Dayyeh, MD1, Eric J. Vargas, MD, MS1
1Mayo Clinic, Rochester, MN; 2Mayo Clinic School of Graduate Medical Education, Rochester, MN; 3Mayo Clinic, Hartford, CT; 4Mayo Clinic, Miami, FL
Introduction: Post procedure hospital admissions & emergency department visits can strain the healthcare system and decrease overall patient satisfaction with endoscopic bariatric procedures. We aim to determine if implementation of a standardized peri-procedural protocol can reduce healthcare utilization.
Methods: All outpatient endoscopic bariatric procedures (intragastric balloon placement(IGB), endoscopic transoral outlet reduction(TORe), endoscopic sleeve gastroplasty(ESG)) between Jan 2012& March 2022 were reviewed. The number of post procedure hospital admissions, emergency department(ED) visits, and infusion therapy center(ITC) visits was collected. Before 2019, patients received post-procedure prescriptions for PO ondansentron, promethazine suppositories, PO pantoprazole, PO acetaminophen and PO opiate for breakthrough pain. In 2019, all patients received a standardized peri-procedure hydration, anti-emetic, and analgesic bundle consisting of intravenous fluids, dexamethasone, ondansentron, acetaminophen, ketorolac, pantoprazole, along with a scopolamine patch and oral aprepitant, the “Enhanced Recovery After Endoscopic ProcedureS” (ERAS) protocol. Patients were also given previously mentioned outpatient regimen without PO opiate and were contacted by a nurse 24-48 hrs post procedure. The number of post-procedure hospital admissions, ED and ITC visits were compared pre & post intervention.
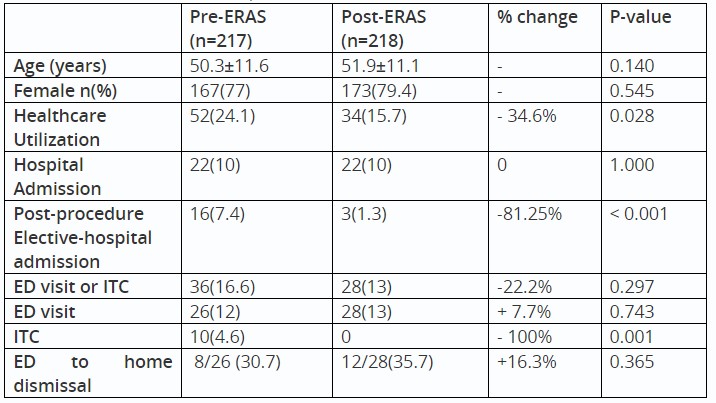
Results: 435 endoscopic bariatric procedures were performed between Jan 2012 and March 2022. The mean age of overall group was 51.1 ± 11.3 and 78.2% were female. N=217 procedures were performed before “ERAS” protocol and N=218 were performed with the protocol in place. Post implementation, overall health care utilization rate decreased from 24.1% to 15.7% (p-value=0.028) while the global hospitalization rate remained the same. The number of post-procedure elective admissions decreased from 7.4% to 1.3%(< 0.001). The overall ED visit rate increased slightly from 12% to 13%, and the ITC visits rate decreased from 4.6% to 0 (0.001). More patients were dismissed from the ED to home with follow up (30.7% vs. 35.7%) over being admitted (Table 1).
Discussion: Implementation of a standardized ERAS protocol for endoscopic bariatric procedures with a structured post-procedure RN contact reduced overall healthcare utilization, post-procedure elective admissions, and ED visits that result in a hospital admission. Strategic ITC use may further decrease ED visits and hospitalization rates.
Disclosures:
Farah Abdul Razzak, MD1, Khushboo Gala, MBBS2, Karim Al Annan, MD3, Razan Aburumman, MD1, Anthony Kerbage, MD1, Rudy Mrad, MD1, Donna Maria Abboud, MD4, Barham Abu Dayyeh, MD1, Eric J. Vargas, MD, MS1, 18, A Quality Improvement Project: The ERAS Protocol Reduces Post Endoscopic Bariatric Procedure Healthcare Utilization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Mayo Clinic School of Graduate Medical Education, Rochester, MN; 3Mayo Clinic, Hartford, CT; 4Mayo Clinic, Miami, FL
Introduction: Post procedure hospital admissions & emergency department visits can strain the healthcare system and decrease overall patient satisfaction with endoscopic bariatric procedures. We aim to determine if implementation of a standardized peri-procedural protocol can reduce healthcare utilization.
Methods: All outpatient endoscopic bariatric procedures (intragastric balloon placement(IGB), endoscopic transoral outlet reduction(TORe), endoscopic sleeve gastroplasty(ESG)) between Jan 2012& March 2022 were reviewed. The number of post procedure hospital admissions, emergency department(ED) visits, and infusion therapy center(ITC) visits was collected. Before 2019, patients received post-procedure prescriptions for PO ondansentron, promethazine suppositories, PO pantoprazole, PO acetaminophen and PO opiate for breakthrough pain. In 2019, all patients received a standardized peri-procedure hydration, anti-emetic, and analgesic bundle consisting of intravenous fluids, dexamethasone, ondansentron, acetaminophen, ketorolac, pantoprazole, along with a scopolamine patch and oral aprepitant, the “Enhanced Recovery After Endoscopic ProcedureS” (ERAS) protocol. Patients were also given previously mentioned outpatient regimen without PO opiate and were contacted by a nurse 24-48 hrs post procedure. The number of post-procedure hospital admissions, ED and ITC visits were compared pre & post intervention.
Results: 435 endoscopic bariatric procedures were performed between Jan 2012 and March 2022. The mean age of overall group was 51.1 ± 11.3 and 78.2% were female. N=217 procedures were performed before “ERAS” protocol and N=218 were performed with the protocol in place. Post implementation, overall health care utilization rate decreased from 24.1% to 15.7% (p-value=0.028) while the global hospitalization rate remained the same. The number of post-procedure elective admissions decreased from 7.4% to 1.3%(< 0.001). The overall ED visit rate increased slightly from 12% to 13%, and the ITC visits rate decreased from 4.6% to 0 (0.001). More patients were dismissed from the ED to home with follow up (30.7% vs. 35.7%) over being admitted (Table 1).
Discussion: Implementation of a standardized ERAS protocol for endoscopic bariatric procedures with a structured post-procedure RN contact reduced overall healthcare utilization, post-procedure elective admissions, and ED visits that result in a hospital admission. Strategic ITC use may further decrease ED visits and hospitalization rates.
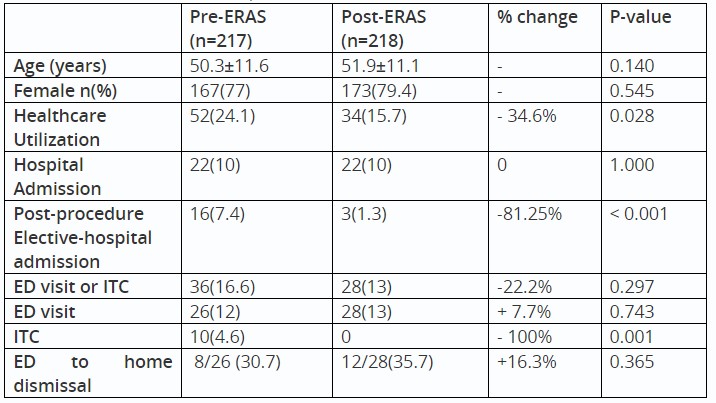
Table: Table 1: Healthcare Utilization Rates Pre and Post "Enhanced Recovery After Endoscopic ProcedureS” (ERAS) Protocol
Disclosures:
Farah Abdul Razzak indicated no relevant financial relationships.
Khushboo Gala indicated no relevant financial relationships.
Karim Al Annan indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Anthony Kerbage indicated no relevant financial relationships.
Rudy Mrad indicated no relevant financial relationships.
Donna Maria Abboud indicated no relevant financial relationships.
Barham Abu Dayyeh indicated no relevant financial relationships.
Eric Vargas: Philips – Grant/Research Support.
Farah Abdul Razzak, MD1, Khushboo Gala, MBBS2, Karim Al Annan, MD3, Razan Aburumman, MD1, Anthony Kerbage, MD1, Rudy Mrad, MD1, Donna Maria Abboud, MD4, Barham Abu Dayyeh, MD1, Eric J. Vargas, MD, MS1, 18, A Quality Improvement Project: The ERAS Protocol Reduces Post Endoscopic Bariatric Procedure Healthcare Utilization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

