Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2A - Small Intestine / Functional / Liver
22 - The Use of Non-Fasting Breath Gas Levels to Predict Response to a FODMAP Restricted Diet
Tuesday, October 29, 2024
9:00 AM - 9:10 AM ET
Location: Terrace Ballroom 1

Prashant Singh, MD
University of Michigan
Ann Arbor, MI
Presenting Author(s)
Prashant Singh, MD1, Robert Burke, MSc2, Barry McBride, MSc3, Claire Shortt, PhD4, William D. Chey, MD, FACG1
1University of Michigan, Ann Arbor, MI; 2FoodMarble Digestive Health Ltd., Tipperary, Tipperary, Ireland; 3FoodMarble Digestive Health Ltd., Dublin, Dublin, Ireland; 4FoodMarble, Dublin, Dublin, Ireland
Introduction: The low fermentable oligo-, di-, monosaccharides and polyols (FODMAP) diet (LFD) is the most evidence-based dietary therapy for patients with irritable bowel syndrome (IBS). However, up to 50% of patients with IBS do not improve with the LFD. This is partly due to a lack of well-defined biomarkers to predict response. Given that excessive colonic fermentation has been linked to symptoms in IBS, in this retrospective analysis of adults with GI symptoms who underwent an app-based LFD self-management program (FoodMarble, Ireland), we interrogated whether pre-intervention, breath patterns were associated with clinical response to the restriction phase of the LFD.
Methods: Self-selected subjects with mild/moderate GI symptoms used an app-connected breath analyzer to collect hourly H2 and CH4 readings during waking hours and logged meal content and symptom severity (0-10 scale). Subjects consumed their habitual diet for 1 week, before following an app-directed LFD for 1 week. Responders were defined as those with a ≥ 30% reduction in at least one mean symptom score (bloating, abdominal pain, flatulence). Baseline average hourly H2 and CH4 levels and symptom scores were compared between LFD responders and non-responders.
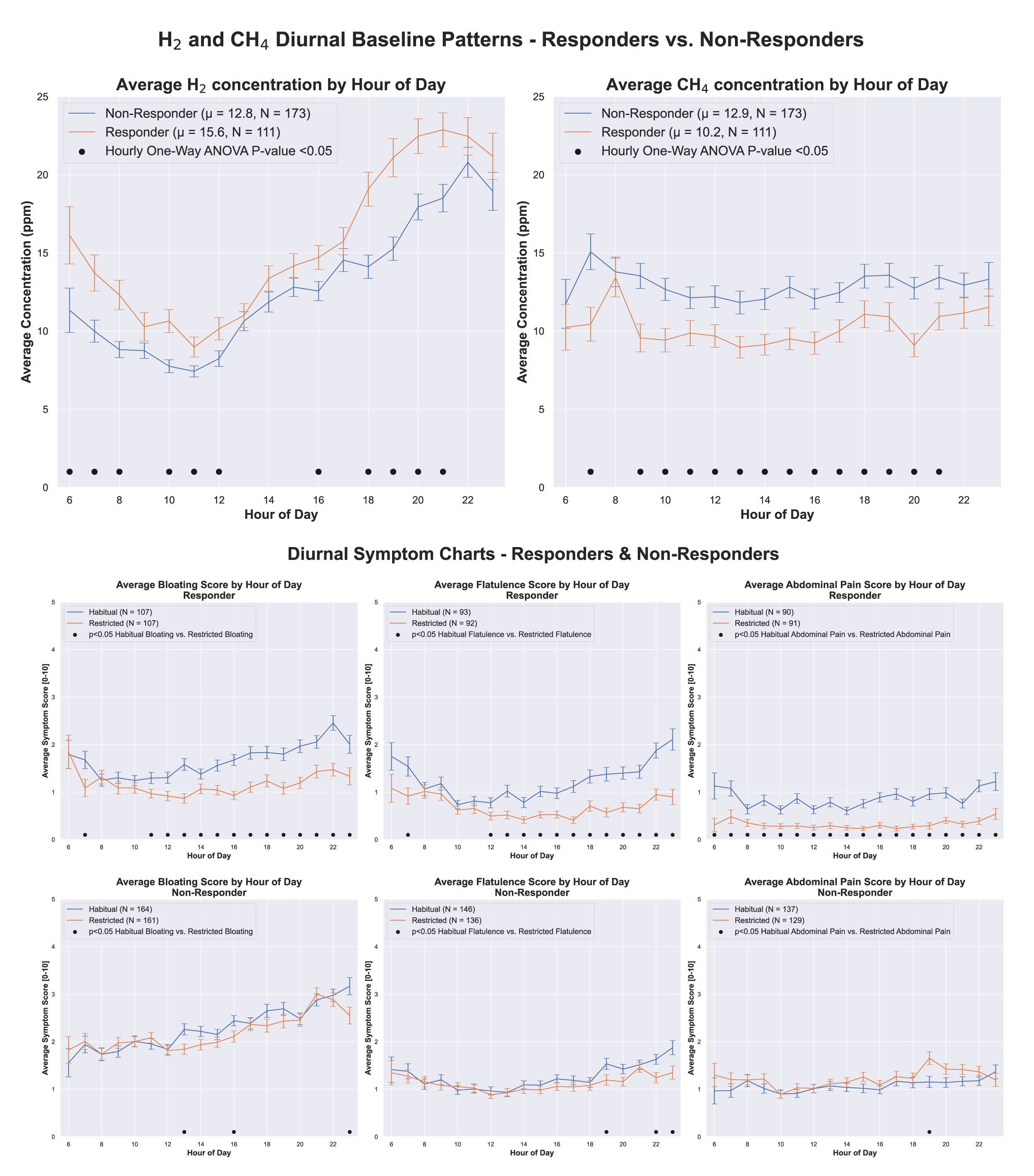
Results: Of 284 subjects (186 women, mean age 45 ± 13), 111 subjects were classified as responders, 173 were classified as non-responders. After FODMAP restriction, LFD responders had consistently lower abdominal pain throughout the day, while bloating and flatulence were lower predominantly in the latter part of the day (Fig. 1). From a prediction perspective, baseline H2 levels were higher among responders compared to non-responders, particularly in the morning and evening. Conversely, responders had lower baseline CH4 levels throughout the day (Fig. 1). LFD responders had lower baseline bloating and abdominal pain scores, with no between group difference in baseline flatulence scores. Average baseline daily FODMAP consumption did not differ significantly between the two groups.
Discussion: Despite comparable FODMAP consumption at baseline, responders to the LFD had higher baseline H2 and lower CH4 levels than non-responders. This suggests a difference in baseline microbiota composition regarding saccharolytic capacity and/or methanogens. Further research is needed to fully characterize and understand these observations. If validated, breath gas patterns might be leveraged as a biomarker to identify responders to the LFD.
Disclosures:
Prashant Singh, MD1, Robert Burke, MSc2, Barry McBride, MSc3, Claire Shortt, PhD4, William D. Chey, MD, FACG1, 22, The Use of Non-Fasting Breath Gas Levels to Predict Response to a FODMAP Restricted Diet, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2FoodMarble Digestive Health Ltd., Tipperary, Tipperary, Ireland; 3FoodMarble Digestive Health Ltd., Dublin, Dublin, Ireland; 4FoodMarble, Dublin, Dublin, Ireland
Introduction: The low fermentable oligo-, di-, monosaccharides and polyols (FODMAP) diet (LFD) is the most evidence-based dietary therapy for patients with irritable bowel syndrome (IBS). However, up to 50% of patients with IBS do not improve with the LFD. This is partly due to a lack of well-defined biomarkers to predict response. Given that excessive colonic fermentation has been linked to symptoms in IBS, in this retrospective analysis of adults with GI symptoms who underwent an app-based LFD self-management program (FoodMarble, Ireland), we interrogated whether pre-intervention, breath patterns were associated with clinical response to the restriction phase of the LFD.
Methods: Self-selected subjects with mild/moderate GI symptoms used an app-connected breath analyzer to collect hourly H2 and CH4 readings during waking hours and logged meal content and symptom severity (0-10 scale). Subjects consumed their habitual diet for 1 week, before following an app-directed LFD for 1 week. Responders were defined as those with a ≥ 30% reduction in at least one mean symptom score (bloating, abdominal pain, flatulence). Baseline average hourly H2 and CH4 levels and symptom scores were compared between LFD responders and non-responders.
Results: Of 284 subjects (186 women, mean age 45 ± 13), 111 subjects were classified as responders, 173 were classified as non-responders. After FODMAP restriction, LFD responders had consistently lower abdominal pain throughout the day, while bloating and flatulence were lower predominantly in the latter part of the day (Fig. 1). From a prediction perspective, baseline H2 levels were higher among responders compared to non-responders, particularly in the morning and evening. Conversely, responders had lower baseline CH4 levels throughout the day (Fig. 1). LFD responders had lower baseline bloating and abdominal pain scores, with no between group difference in baseline flatulence scores. Average baseline daily FODMAP consumption did not differ significantly between the two groups.
Discussion: Despite comparable FODMAP consumption at baseline, responders to the LFD had higher baseline H2 and lower CH4 levels than non-responders. This suggests a difference in baseline microbiota composition regarding saccharolytic capacity and/or methanogens. Further research is needed to fully characterize and understand these observations. If validated, breath gas patterns might be leveraged as a biomarker to identify responders to the LFD.
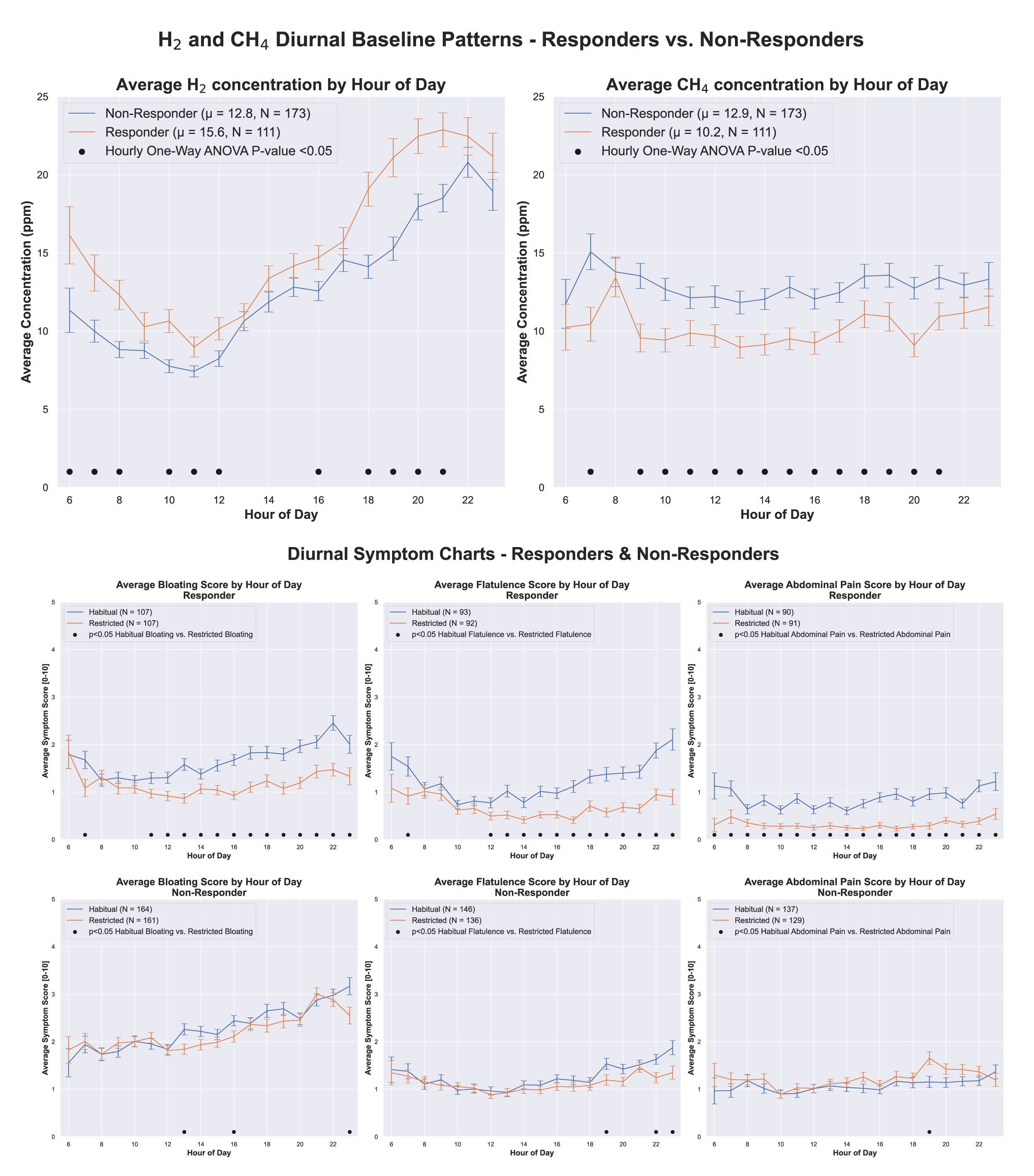
Figure: Non-fasting breath hydrogen and methane levels patterns at baseline and in response to low FODMAP diet
Disclosures:
Prashant Singh: Uptodate – Royalties.
Robert Burke: FoodMarble Digestive Health – Employee.
Barry McBride: FoodMarble Digestive Health – Employee.
Claire Shortt: FoodMarble Digestive Health – Employee.
William Chey: AbbVie – Consultant. Ardelyx – Consultant. Atmo BioSciences – Consultant. Comvita – Consultant. Corprata – Stock Options. Dieta Health – Stock Options. FoodMarble Digestive Health – Consultant, Stock Options. Ironwood Pharmaceuticals – Consultant. Modify Health – Stock Options. Nestlé S.A. – Consultant. Phathom Pharmaceuticals – Consultant. Redhill Biopharma – Consultant. Salix Pharmaceuticals – Consultant. Takeda – Consultant. Vibrant Gastro – Consultant.
Prashant Singh, MD1, Robert Burke, MSc2, Barry McBride, MSc3, Claire Shortt, PhD4, William D. Chey, MD, FACG1, 22, The Use of Non-Fasting Breath Gas Levels to Predict Response to a FODMAP Restricted Diet, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

