Tuesday Poster Session
Category: IBD
P4398 - The Impact of Mirikizumab Induction, Maintenance, and Long-Term Treatment on Disease Clearance in Patients With Moderately to Severely Active Ulcerative Colitis: Post-Hoc Analysis of LUCENT Trials
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JW
Jianmin Wu
Eli Lilly and Company
Indianapolis, IN
Presenting Author(s)
Jean-Frédéric Colombel, MD1, Taku Kobayashi, MD2, Jianmin Wu, 3, Baojin Zhu, 3, Vipul Jairath, MBChB4, Isabel Redondo, MD5, Richard Moses, 3, Corey A.. Siegel, MD, MS6, Britta Siegmund, MD7, Fernando Magro, 8
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Kitasato University Kitasato Institute Hospital, Minato City, Tokyo, Japan; 3Eli Lilly and Company, Indianapolis, IN; 4Western University, London, ON, Canada; 5Eli Lilly and Company, Lisboa, Lisboa, Portugal; 6Dartmouth-Hitchcock Medical Center, Lebanon, NH; 7Med. Klinik für Gastroenterologie, Infektiologie, Rheumatologie, Charité – Universitätsmedizin Berlin, Freie Universität Berlin, Humboldt-Universität zu Berlin, Campus Benjamin Franklin, Hindenburgdamm, Berlin, Germany; 8Centro Hospitalar São João, Porto, Porto, Portugal
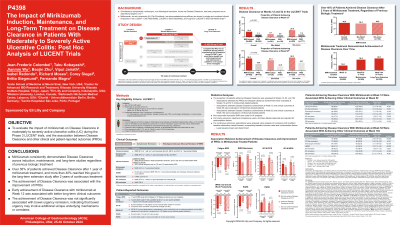
Introduction: Disease clearance (DC) has been proposed as an aspirational target in ulcerative colitis (UC). Mirikizumab (miri) has demonstrated strong efficacy in LUCENT Phase 3 trials. This analysis evaluated the impact of miri on DC during LUCENT-1, -2 and long-term LUCENT-3 trials and the association between DC and other clinical and patient-reported outcomes (PROs).
Methods: DC: symptomatic remission [Mayo stool frequency (SF)=0, 1 with ≥1 point decrease from baseline + rectal bleeding (RB)=0] and histologic-endoscopic mucosal remission [HEMR: Mayo endoscopic remission (ER: endoscopy subscore of 0 or 1, excluding friability) + Geboes score ≤2B.0]. PROs: Fatigue NRS, IBDQ remission, SF-36, WPAI:UC, PGRS and PGRC (see table footer). Clinical outcomes: clinical remission, corticosteroid-free remission, ER, HEMR, bowel urgency (BU) remission, SF remission and RB remission. Patient proportion achieving DC was assessed at W12, 52 and 104. Associations between the PROs and DC were evaluated at W12 and 52 and those between clinical outcomes and early DC achievement in miri-treated patients at W12 and W52 were evaluated at W52 and W104, respectively.
Results: Significantly higher proportion of miri-treated patients achieved DC vs PBO at W12 (N=868 miri, 294 PBO; DC: 16.0% vs 7.1%, p< 0.0001) and W52 (N=365 miri, 179 PBO; DC: 36.4% vs 19.6%, p=0.0002). Similar trends were seen for biologic failure subgroups at W12 (bio/JAKi-failed DC: 9.1% miri vs 5.9% PBO; bio&JAKi-naïve DC: 20.9% miri vs 7.6% PBO) and W52 (bio/JAKi-failed DC: 31.3% miri vs 12.5% PBO; bio&JAKi-naïve DC: 39.3% miri vs 23.7% PBO). At W104 (N=239 miri), 40.6% patients achieved DC with 2-year of treatment. 38.4% bio/JAKi-failed (n=73) and 40.9% bio&JAKi-naïve (n=159) patients achieved DC. Significantly greater improvement in all PROs was seen at W12 for miri-treated patients who achieved DC vs those who did not at W12. Similar associations were observed at W52, except in WPAI: UC overall work productivity (Table-1A). Patients achieving DC at W12 were more likely to achieve all clinical outcomes, except BU remission, at W52 vs those who did not achieve W12 DC. This trend repeated in those who achieved DC at W52 and continued to W104 (Table-1B).
Discussion: Miri consistently demonstrated DC across induction, maintenance and long-term studies. Over 36% patients achieved DC after one year of miri treatment. DC attainment was associated with improvement in PROs in LUCENT-1 and -2. Early DC was associated with better long-term clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jean-Frédéric Colombel, MD1, Taku Kobayashi, MD2, Jianmin Wu, 3, Baojin Zhu, 3, Vipul Jairath, MBChB4, Isabel Redondo, MD5, Richard Moses, 3, Corey A.. Siegel, MD, MS6, Britta Siegmund, MD7, Fernando Magro, 8. P4398 - The Impact of Mirikizumab Induction, Maintenance, and Long-Term Treatment on Disease Clearance in Patients With Moderately to Severely Active Ulcerative Colitis: Post-Hoc Analysis of LUCENT Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Kitasato University Kitasato Institute Hospital, Minato City, Tokyo, Japan; 3Eli Lilly and Company, Indianapolis, IN; 4Western University, London, ON, Canada; 5Eli Lilly and Company, Lisboa, Lisboa, Portugal; 6Dartmouth-Hitchcock Medical Center, Lebanon, NH; 7Med. Klinik für Gastroenterologie, Infektiologie, Rheumatologie, Charité – Universitätsmedizin Berlin, Freie Universität Berlin, Humboldt-Universität zu Berlin, Campus Benjamin Franklin, Hindenburgdamm, Berlin, Germany; 8Centro Hospitalar São João, Porto, Porto, Portugal
Introduction: Disease clearance (DC) has been proposed as an aspirational target in ulcerative colitis (UC). Mirikizumab (miri) has demonstrated strong efficacy in LUCENT Phase 3 trials. This analysis evaluated the impact of miri on DC during LUCENT-1, -2 and long-term LUCENT-3 trials and the association between DC and other clinical and patient-reported outcomes (PROs).
Methods: DC: symptomatic remission [Mayo stool frequency (SF)=0, 1 with ≥1 point decrease from baseline + rectal bleeding (RB)=0] and histologic-endoscopic mucosal remission [HEMR: Mayo endoscopic remission (ER: endoscopy subscore of 0 or 1, excluding friability) + Geboes score ≤2B.0]. PROs: Fatigue NRS, IBDQ remission, SF-36, WPAI:UC, PGRS and PGRC (see table footer). Clinical outcomes: clinical remission, corticosteroid-free remission, ER, HEMR, bowel urgency (BU) remission, SF remission and RB remission. Patient proportion achieving DC was assessed at W12, 52 and 104. Associations between the PROs and DC were evaluated at W12 and 52 and those between clinical outcomes and early DC achievement in miri-treated patients at W12 and W52 were evaluated at W52 and W104, respectively.
Results: Significantly higher proportion of miri-treated patients achieved DC vs PBO at W12 (N=868 miri, 294 PBO; DC: 16.0% vs 7.1%, p< 0.0001) and W52 (N=365 miri, 179 PBO; DC: 36.4% vs 19.6%, p=0.0002). Similar trends were seen for biologic failure subgroups at W12 (bio/JAKi-failed DC: 9.1% miri vs 5.9% PBO; bio&JAKi-naïve DC: 20.9% miri vs 7.6% PBO) and W52 (bio/JAKi-failed DC: 31.3% miri vs 12.5% PBO; bio&JAKi-naïve DC: 39.3% miri vs 23.7% PBO). At W104 (N=239 miri), 40.6% patients achieved DC with 2-year of treatment. 38.4% bio/JAKi-failed (n=73) and 40.9% bio&JAKi-naïve (n=159) patients achieved DC. Significantly greater improvement in all PROs was seen at W12 for miri-treated patients who achieved DC vs those who did not at W12. Similar associations were observed at W52, except in WPAI: UC overall work productivity (Table-1A). Patients achieving DC at W12 were more likely to achieve all clinical outcomes, except BU remission, at W52 vs those who did not achieve W12 DC. This trend repeated in those who achieved DC at W52 and continued to W104 (Table-1B).
Discussion: Miri consistently demonstrated DC across induction, maintenance and long-term studies. Over 36% patients achieved DC after one year of miri treatment. DC attainment was associated with improvement in PROs in LUCENT-1 and -2. Early DC was associated with better long-term clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jean-Frédéric Colombel: AbbVie – Consultant, Grant/Research Support. Allergan – Consultant. Amgen – Consultant. AnaptysBio – Consultant. Arena Pharmaceuticals – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squib – Consultant, Grant/Research Support. Celgene – Consultant. Celltrion – Consultant. Eli Lilly – Consultant. Enterome – Consultant. Ferring – Consultant. Galmed Research – Consultant. Genentech – Consultant. Genfit – Stock-publicly held company(excluding mutual/index funds). Glaxo Smith Kline – Consultant. Immunic – Consultant. Intestinal Biotech Development – Stock-publicly held company(excluding mutual/index funds). Iterative Scopes – Consultant. Janssen – Consultant, Grant/Research Support. Johnson & Johnson – Consultant, Grant/Research Support. Kaleido Biosciences – Consultant. Landos – Consultant. MedImmune – Consultant. Merck – Consultant. Microba Life Science – Consultant. Novartis – Consultant. Otsuka Pharmaceutical – Consultant. Pfizer – Consultant. PPM Services – Consultant. Protagonist – Consultant. Sanofi – Consultant. Second Genome – Consultant. Seres – Consultant. Shire – Consultant. Takeda – Consultant, Grant/Research Support. Theradiag – Consultant. TiGenix – Consultant. Vifor – Consultant.
Taku Kobayashi: AbbVie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Alfresa Pharma – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Alimentiv – Advisory Committee/Board Member, Consultant, Speakers Bureau. Astellas – Advisory Committee/Board Member, Consultant, Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speakers Bureau. Celltrion – Advisory Committee/Board Member, Consultant, Speakers Bureau. Covidien – Advisory Committee/Board Member, Consultant, Speakers Bureau. EA Pharma – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Consultant, Speakers Bureau. Ferring – Advisory Committee/Board Member, Consultant, Speakers Bureau. Galapagos – Advisory Committee/Board Member, Consultant, Speakers Bureau. Gilead Sciences – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. JIMRO – Advisory Committee/Board Member, Consultant, Speakers Bureau. JMDC – Advisory Committee/Board Member, Consultant, Speakers Bureau. Kissei Pharmaceutical – Advisory Committee/Board Member, Consultant, Speakers Bureau. Kyorin Pharmaceutical – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Mitsubishi Tanabe Pharma – Advisory Committee/Board Member, Consultant, Speakers Bureau. Mochida Pharmaceutical – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Nippon Kayaku – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Otsuka Holdings – Grant/Research Support. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Sekisui Medical – Grant/Research Support. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. ThermoFisher Scientific – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Zeria Pharmaceutical – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau.
Jianmin Wu: Eli Lilly and Company – Employee, Stock Options.
Baojin Zhu: Eli Lilly and Company – Employee, Stock Options.
Vipul Jairath: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. Alimentiv – Consultant, Employee, Grant/Research Support, Speakers Bureau. Arena Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Asahi Kasei Pharma – Consultant, Grant/Research Support, Speakers Bureau. Asieris Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. AstraZeneca – Consultant, Grant/Research Support, Speakers Bureau. Avoro Capital – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support, Speakers Bureau. Celltrion – Consultant, Grant/Research Support, Speakers Bureau. Eli Lilly and Company – Consultant, Grant/Research Support, Speakers Bureau. Endpoint Health – Advisory Committee/Board Member, Consultant. Enthera – Advisory Committee/Board Member, Consultant. Ferring Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Flagship Pioneering – Consultant, Grant/Research Support, Speakers Bureau. Fresenius Kabi – Consultant, Grant/Research Support, Speakers Bureau. Galapagos NV – Consultant, Grant/Research Support, Speakers Bureau. Genentech – Consultant, Grant/Research Support, Speakers Bureau. Gilde Healthcare – Advisory Committee/Board Member, Consultant. Gilead Sciences – Consultant, Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Consultant, Grant/Research Support, Speakers Bureau. Innomar – Advisory Committee/Board Member, Consultant. JAMP – Advisory Committee/Board Member, Consultant. Janssen – Consultant, Grant/Research Support, Speakers Bureau. London Health Sciences Centre – Employee. Merck – Consultant, Grant/Research Support, Speakers Bureau. Metacrine – Consultant, Grant/Research Support, Speakers Bureau. Mylan – Consultant, Grant/Research Support, Speakers Bureau. Pandion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Pendopharm – Consultant, Grant/Research Support, Speakers Bureau. Pfizer – Consultant, Grant/Research Support, Speakers Bureau. Prometheus Therapeutics and Diagnostics – Consultant, Grant/Research Support, Speakers Bureau. Protagonist Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Reistone Biopharma – Consultant, Grant/Research Support, Speakers Bureau. Roche – Consultant, Grant/Research Support, Speakers Bureau. Roivant – Advisory Committee/Board Member, Consultant. Sandoz – Consultant, Grant/Research Support, Speakers Bureau. SCOPE – Advisory Committee/Board Member, Consultant. Second Genome – Consultant, Grant/Research Support, Speakers Bureau. Shire – Speakers Bureau. Sorriso Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Synedgen – Advisory Committee/Board Member, Consultant. Takeda – Consultant, Grant/Research Support, Speakers Bureau. TD Securities – Advisory Committee/Board Member, Consultant. Teva – Consultant, Grant/Research Support, Speakers Bureau. Topivert – Consultant, Grant/Research Support, Speakers Bureau. Ventyx Biosciences – Consultant, Grant/Research Support, Speakers Bureau. Vividion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau.
Isabel Redondo: ELLI LILLY – Employee, Stock Options.
Richard Moses: Eli Lilly and Company – Employee, Stock Options.
Corey Siegel: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker for CME activities. BMS – Advisory Committee/Board Member, Consultant. Boomerang – Advisory Committee/Board Member, Consultant. Buhlman – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker for CME activities. Lilly – Advisory Committee/Board Member, Consultant. Napo pharmaceuticals – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Prometheus Labs – Advisory Committee/Board Member, Consultant. Roivant – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Trellus Health – Advisory Committee/Board Member, Consultant.
Britta Siegmund: AbbVie – Consultant, Speakers Bureau. Arena Pharmaceuticals – Consultant, Speakers Bureau. Boehringer Ingelheim – Consultant, Speakers Bureau. Bristol Myers Squibb – Consultant, Speakers Bureau. CED Service GmbH – Consultant, Speakers Bureau. Celgene – Consultant, Speakers Bureau. Dr. Falk Pharma – Consultant, Speakers Bureau. Eli Lilly and Company – Consultant, Grant/Research Support, Speakers Bureau. Ferring Pharmaceuticals – Consultant, Speakers Bureau. Galapagos NV – Consultant, Speakers Bureau. Janssen – Consultant, Speakers Bureau. Novartis – Consultant, Speakers Bureau. Pfizer – Consultant, Speakers Bureau. Prometheus Therapeutics – Consultant, Speakers Bureau. Takeda – Consultant, Speakers Bureau.
Fernando Magro: AbbVie – Received honoraria, Speakers Bureau. Biogen – Received honoraria, Speakers Bureau. Dr. Falk Pharma – Received honoraria. Ferring Pharmaceuticals – Received honoraria, Speakers Bureau. Hospira – Received honoraria, Speakers Bureau. Laboratórios Vitória – Received honoraria, Speakers Bureau. Merck Sharp & Dohme – Received honoraria, Speakers Bureau. Vifor Pharma – Received honoraria, Speakers Bureau.
Jean-Frédéric Colombel, MD1, Taku Kobayashi, MD2, Jianmin Wu, 3, Baojin Zhu, 3, Vipul Jairath, MBChB4, Isabel Redondo, MD5, Richard Moses, 3, Corey A.. Siegel, MD, MS6, Britta Siegmund, MD7, Fernando Magro, 8. P4398 - The Impact of Mirikizumab Induction, Maintenance, and Long-Term Treatment on Disease Clearance in Patients With Moderately to Severely Active Ulcerative Colitis: Post-Hoc Analysis of LUCENT Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
