Tuesday Poster Session
Category: IBD
P4453 - Immediate Hypersensitivity to Intravenous Risankizumab-Rzaa but Subsequent Tolerance to Subcutaneous Risankizumab-Rzaa
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jeremy A. Klein, MD (he/him/his)
University of Chicago Medical Center
Chicago, IL
Presenting Author(s)
Jeremy A. Klein, MD1, David T. Choi, PharmD2, Benjamin D. McDonald, MD, PhD2, David T.. Rubin, MD, FACG2
1University of Chicago Medical Center, Chicago, IL; 2University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL
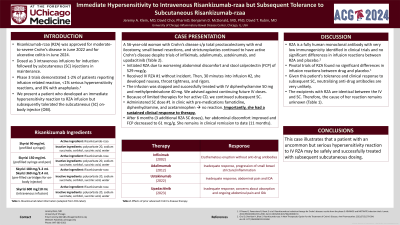
Introduction: Risankizumab-rzaa (RZA) is approved for moderate-to-severe Crohn’s disease (CD) and is dosed three intravenous (IV) infusions for induction followed by subcutaneous (SC) injections in maintenance. Phase 3 trials demonstrated the safety of IV RZA with 1-2% reporting infusion related reaction, < 1% serious hypersensitivity reactions, and 0% with anaphylaxis. We present a patient who developed an immediate hypersensitivity reaction to RZA infusion but subsequently tolerated the subcutaneous (SC) on-body injector (OBI).
Case Description/Methods: The patient is a 56-year-old woman with CD who required total proctocolectomy with end ileostomy and subsequent small bowel resections and stricturoplasties. Prior therapies included infliximab (developed erythematous eruption without anti-drug antibodies), and inadequate response to adalimumab, ustekinumab, and upadacitinib. RZA was prescribed due to worsening abdominal discomfort and stool calprotectin (FCP) of 529 mcg/g. She received the first IV RZA without incident. However, 30 minutes into the second infusion, she developed nausea, throat tightness, and rigors. The infusion was stopped and she was treated successfully with IV diphenhydramine 50 mg and methylprednisolone 40 mg. Because of limited remaining therapies for her active CD, we decided to forego the remaining IV doses and continue SC formulation. She administered the first SC dose with pre-medications famotidine, diphenhydramine, and acetaminophen and had no reaction. Importantly, she had a clinical response to therapy. After 6 months (3 additional RZA SC doses), her abdominal discomfort improved and FCP improved to 61 mcg/g. She has not used premedication since the first SC dose and has received 2 additional doses.
Discussion: RZA is a fully human monoclonal antibody with very low immunogenicity identified in clinical trials, and no significant differences in infusion reactions between drug and placebo. Given this patient’s tolerance and clinical response to subsequent SC, neutralizing anti-drug antibodies are very unlikely. The excipients with RZA are identical between the IV and SC, so the cause of her reaction remains unknown. Similarly, we first reported hypersensitivity with one dose of IV ustekinumab with subsequent tolerance of SC, but hypothesized this may be due to IV ustekinumab containing EDTA while SC does not. This case illustrates that a patient with an uncommon but serious hypersensitivity reaction to IV RZA may be safely and successfully transitioned to SC dosing.
Disclosures:
Jeremy A. Klein, MD1, David T. Choi, PharmD2, Benjamin D. McDonald, MD, PhD2, David T.. Rubin, MD, FACG2. P4453 - Immediate Hypersensitivity to Intravenous Risankizumab-Rzaa but Subsequent Tolerance to Subcutaneous Risankizumab-Rzaa, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Chicago Medical Center, Chicago, IL; 2University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL
Introduction: Risankizumab-rzaa (RZA) is approved for moderate-to-severe Crohn’s disease (CD) and is dosed three intravenous (IV) infusions for induction followed by subcutaneous (SC) injections in maintenance. Phase 3 trials demonstrated the safety of IV RZA with 1-2% reporting infusion related reaction, < 1% serious hypersensitivity reactions, and 0% with anaphylaxis. We present a patient who developed an immediate hypersensitivity reaction to RZA infusion but subsequently tolerated the subcutaneous (SC) on-body injector (OBI).
Case Description/Methods: The patient is a 56-year-old woman with CD who required total proctocolectomy with end ileostomy and subsequent small bowel resections and stricturoplasties. Prior therapies included infliximab (developed erythematous eruption without anti-drug antibodies), and inadequate response to adalimumab, ustekinumab, and upadacitinib. RZA was prescribed due to worsening abdominal discomfort and stool calprotectin (FCP) of 529 mcg/g. She received the first IV RZA without incident. However, 30 minutes into the second infusion, she developed nausea, throat tightness, and rigors. The infusion was stopped and she was treated successfully with IV diphenhydramine 50 mg and methylprednisolone 40 mg. Because of limited remaining therapies for her active CD, we decided to forego the remaining IV doses and continue SC formulation. She administered the first SC dose with pre-medications famotidine, diphenhydramine, and acetaminophen and had no reaction. Importantly, she had a clinical response to therapy. After 6 months (3 additional RZA SC doses), her abdominal discomfort improved and FCP improved to 61 mcg/g. She has not used premedication since the first SC dose and has received 2 additional doses.
Discussion: RZA is a fully human monoclonal antibody with very low immunogenicity identified in clinical trials, and no significant differences in infusion reactions between drug and placebo. Given this patient’s tolerance and clinical response to subsequent SC, neutralizing anti-drug antibodies are very unlikely. The excipients with RZA are identical between the IV and SC, so the cause of her reaction remains unknown. Similarly, we first reported hypersensitivity with one dose of IV ustekinumab with subsequent tolerance of SC, but hypothesized this may be due to IV ustekinumab containing EDTA while SC does not. This case illustrates that a patient with an uncommon but serious hypersensitivity reaction to IV RZA may be safely and successfully transitioned to SC dosing.
Disclosures:
Jeremy Klein indicated no relevant financial relationships.
David Choi: AbbVie – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Eli Lilly – Consultant, Speakers Bureau. Janssen Pharmaceuticals – Consultant, Speakers Bureau.
Benjamin McDonald indicated no relevant financial relationships.
David Rubin: AbbVie – Consultant. AltruBio – Consultant. Apex – Consultant. Avalo Therapeutics – Consultant. Bausch Health – Consultant. Bristol Myers Squibb – Consultant. Buhlmann Diagnostics Corp – Consultant. Celgene – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health – Board of Directors. Crohn's & Colitis Foundation – Board of Trustees. Douglas Therapeutics – Consultant. Eli Lilly – Consultant. InDex Pharmaceuticals – Consultant. Intouch Group – Consultant. Iterative Health – Consultant. Janssen Pharmaceuticals – Consultant. Odyssey Thera – Consultant. Pfizer – Consultant. Prometheus Biosciences – Consultant. Samsung Neurologica – Consultant. Takeda – Consultant, Grant/Research Support.
Jeremy A. Klein, MD1, David T. Choi, PharmD2, Benjamin D. McDonald, MD, PhD2, David T.. Rubin, MD, FACG2. P4453 - Immediate Hypersensitivity to Intravenous Risankizumab-Rzaa but Subsequent Tolerance to Subcutaneous Risankizumab-Rzaa, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

