Tuesday Poster Session
Category: Interventional Endoscopy
P4554 - Navigating Complex Esophageal Perforations: A Case-Specific Approach to Successful Outcomes
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Harsimran Kalsi, MBBS (she/her/hers)
University of Central Florida College of Medicine
Gainesville, FL
Presenting Author(s)
Harsimran Kalsi, MBBS1, Kobina Essilfie-Quaye, MD1, Mohammad Abuassi, MD1, Raghav Bassi, MD1, Yaseen Perbtani, DO2, Tony S.. Brar, MD1
1University of Central Florida College of Medicine, Gainesville, FL; 2University of Central Florida, HCA Healthcare GME, Gainesville, FL
Introduction: Esophageal perforation can be a life-threatening condition with mortality rates ranging from 10-60%. Mortality can be significantly improved with timely management. This case details an esophageal perforation that occurred post-leiomyoma enucleation. We highlight not only the challenges involved but also our innovations in endoscopic management.
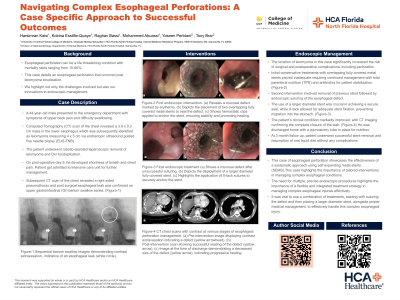
Case Description/Methods: A 44-year-old male presented with symptoms of upper back pain and difficulty swallowing. Computed Tomography (CT) scan chest revealed a 3.8 x 3.3 cm mass in the lower esophagus, which was subsequently identified as a leiomyoma measuring 4 x 5 cm via endoscopic ultrasound-guided fine needle biopsy (EUS-FNB). The patient underwent robotic-assisted laparoscopic removal of the leiomyoma and Dor fundoplication. However, on postoperative day 5, he developed shortness of breath and chest pain, and CT scan confirmed a right-sided pneumothorax and a postsurgical esophageal leak.
Initial management of the esophageal leak involved primary endoluminal stenting using two overlapping fully covered metal stents (20 mm x 10 cm and 20 mm x 8 cm), which failed to seal the leak on repeat imaging. A subsequent endoscopy led to the removal of these stents, followed by closure of the perforation using the OverStitch endoscopic suturing device. To ensure robust coverage and stabilization, a larger diameter fully covered EndoMAXX stent (23 mm x 100 mm) was placed over the sutured defect. The stent’s position was secured with the X-tack device. Further imaging a few days later confirmed the complete sealing of the leak. The patient's clinical condition markedly improved, with imaging confirming the complete closure of the leak.
Discussion: In this case, the location of leiomyoma significantly increased the risk of surgical and postoperative complications, including perforation. Initial conservative treatments with overlapping fully covered metal stents proved inadequate. Total parenteral nutrition (TPN) and antibiotics stabilized the patient, but further endoscopic therapy was necessary. Advances in endoscopic techniques enabled the effective suturing of the defect. Importantly, the use of a larger diameter stent was crucial for achieving a secure seal. The X-tack device also played a pivotal role in ensuring the stent remained properly positioned, preventing migration into the stomach. This case highlights the importance of tailored interventions in managing complex esophageal conditions.
Disclosures:
Harsimran Kalsi, MBBS1, Kobina Essilfie-Quaye, MD1, Mohammad Abuassi, MD1, Raghav Bassi, MD1, Yaseen Perbtani, DO2, Tony S.. Brar, MD1. P4554 - Navigating Complex Esophageal Perforations: A Case-Specific Approach to Successful Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Central Florida College of Medicine, Gainesville, FL; 2University of Central Florida, HCA Healthcare GME, Gainesville, FL
Introduction: Esophageal perforation can be a life-threatening condition with mortality rates ranging from 10-60%. Mortality can be significantly improved with timely management. This case details an esophageal perforation that occurred post-leiomyoma enucleation. We highlight not only the challenges involved but also our innovations in endoscopic management.
Case Description/Methods: A 44-year-old male presented with symptoms of upper back pain and difficulty swallowing. Computed Tomography (CT) scan chest revealed a 3.8 x 3.3 cm mass in the lower esophagus, which was subsequently identified as a leiomyoma measuring 4 x 5 cm via endoscopic ultrasound-guided fine needle biopsy (EUS-FNB). The patient underwent robotic-assisted laparoscopic removal of the leiomyoma and Dor fundoplication. However, on postoperative day 5, he developed shortness of breath and chest pain, and CT scan confirmed a right-sided pneumothorax and a postsurgical esophageal leak.
Initial management of the esophageal leak involved primary endoluminal stenting using two overlapping fully covered metal stents (20 mm x 10 cm and 20 mm x 8 cm), which failed to seal the leak on repeat imaging. A subsequent endoscopy led to the removal of these stents, followed by closure of the perforation using the OverStitch endoscopic suturing device. To ensure robust coverage and stabilization, a larger diameter fully covered EndoMAXX stent (23 mm x 100 mm) was placed over the sutured defect. The stent’s position was secured with the X-tack device. Further imaging a few days later confirmed the complete sealing of the leak. The patient's clinical condition markedly improved, with imaging confirming the complete closure of the leak.
Discussion: In this case, the location of leiomyoma significantly increased the risk of surgical and postoperative complications, including perforation. Initial conservative treatments with overlapping fully covered metal stents proved inadequate. Total parenteral nutrition (TPN) and antibiotics stabilized the patient, but further endoscopic therapy was necessary. Advances in endoscopic techniques enabled the effective suturing of the defect. Importantly, the use of a larger diameter stent was crucial for achieving a secure seal. The X-tack device also played a pivotal role in ensuring the stent remained properly positioned, preventing migration into the stomach. This case highlights the importance of tailored interventions in managing complex esophageal conditions.
Disclosures:
Harsimran Kalsi indicated no relevant financial relationships.
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Mohammad Abuassi indicated no relevant financial relationships.
Raghav Bassi indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Harsimran Kalsi, MBBS1, Kobina Essilfie-Quaye, MD1, Mohammad Abuassi, MD1, Raghav Bassi, MD1, Yaseen Perbtani, DO2, Tony S.. Brar, MD1. P4554 - Navigating Complex Esophageal Perforations: A Case-Specific Approach to Successful Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
