Tuesday Poster Session
Category: Liver
P4595 - Quality Improvement in Decompensated Cirrhosis: Standardizing the Admission Process
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- LL
Laura E. Lavette, MD (she/her/hers)
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Laura E. Lavette, MD, Hannah Laird, MD, Mira Sridharan, , Jessica Dreicer, MD, Andrew Barros, MD, Kyle Enfield, MD, Zachary Henry, MD
University of Virginia Medical Center, Charlottesville, VA
Introduction: Patients with decompensated cirrhosis have severe underlying disease, leading to increased hospitalizations. Previous Quality Improvement (QI) projects have shown that standardized order sets are associated with decreased re-admissions, medical errors, and mortality.1 We performed a review of patients with decompensated cirrhosis and identified key areas for improvement at time of admission. Based on our findings, we generated an admission order set with the aim to 1) streamline provider’s practice, 2) encourage evidence-based medicine, and 3) improve patient outcomes.
Methods: We performed a retrospective review of patients from 1/1/22 to 9/1/23 at a single tertiary care center. All patients had a diagnosis of decompensated cirrhosis prior to admission. We used findings from our pre-intervention data along with evidence-based practice guidelines to construct a cirrhosis admission order set for providers to use at time of admission or at any point during a patient’s hospitalization.
Results: 229 patients met inclusion criteria. 156 (68%) were admitted to General Medicine and 73 (32%) to the Intensive Care Unit. 123 (54%) received a diagnostic paracentesis during current hospitalization; the average time from admission to paracentesis was 7.5 hours. The average time to collection of MELD labs was 8 hours. 134 (59%) were started on an appropriate cirrhosis diet inpatient. 41 (18%) died or were converted to hospice.
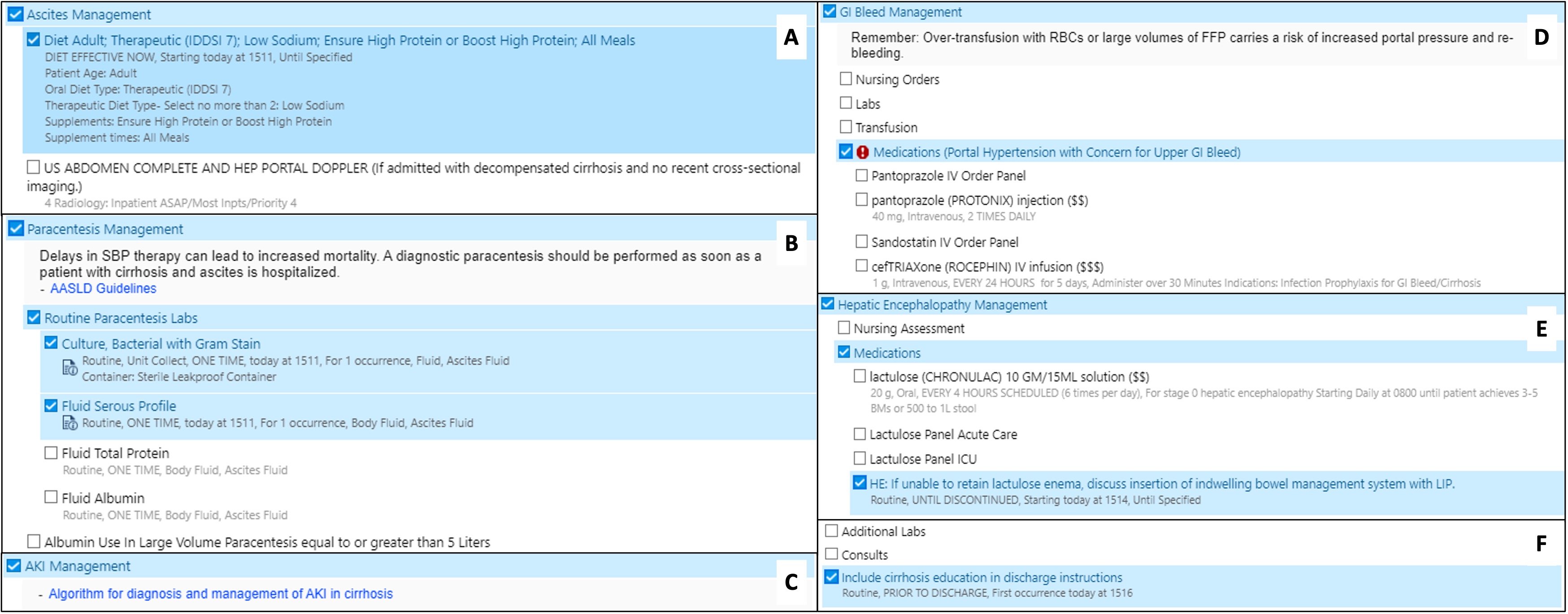
Our order set, “Cirrhosis Management Panel,” was created as a stand-alone order set and was embedded in the “General Admission” order set. It consisted of 8 categories, many being common complications of portal hypertension (Figure 1). Pre-selected categories included diet, paracentesis labs, and cirrhosis education. The remainder of the categories were not automatically selected and left to user discretion.
Discussion: QI efforts have been shown to standardize care between providers and across medical systems. We created an admission order set tailored towards patients with decompensated cirrhosis with the goal of optimizing evidence-based, quality care. Future work will include collecting post-intervention data to evaluate the order set’s impact on patient outcomes. We believe our order set is generalizable to other institutions and is important in encouraging conversations about how to promote QI within the cirrhosis population.
1. Wells C, et al. Standardized Hospital Order Sets in Acute Care: A Review of Clinical Evidence, Cost-Effectiveness, and Guidelines. CADTH; 2019.
Disclosures:
Laura E. Lavette, MD, Hannah Laird, MD, Mira Sridharan, , Jessica Dreicer, MD, Andrew Barros, MD, Kyle Enfield, MD, Zachary Henry, MD. P4595 - Quality Improvement in Decompensated Cirrhosis: Standardizing the Admission Process, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Virginia Medical Center, Charlottesville, VA
Introduction: Patients with decompensated cirrhosis have severe underlying disease, leading to increased hospitalizations. Previous Quality Improvement (QI) projects have shown that standardized order sets are associated with decreased re-admissions, medical errors, and mortality.1 We performed a review of patients with decompensated cirrhosis and identified key areas for improvement at time of admission. Based on our findings, we generated an admission order set with the aim to 1) streamline provider’s practice, 2) encourage evidence-based medicine, and 3) improve patient outcomes.
Methods: We performed a retrospective review of patients from 1/1/22 to 9/1/23 at a single tertiary care center. All patients had a diagnosis of decompensated cirrhosis prior to admission. We used findings from our pre-intervention data along with evidence-based practice guidelines to construct a cirrhosis admission order set for providers to use at time of admission or at any point during a patient’s hospitalization.
Results: 229 patients met inclusion criteria. 156 (68%) were admitted to General Medicine and 73 (32%) to the Intensive Care Unit. 123 (54%) received a diagnostic paracentesis during current hospitalization; the average time from admission to paracentesis was 7.5 hours. The average time to collection of MELD labs was 8 hours. 134 (59%) were started on an appropriate cirrhosis diet inpatient. 41 (18%) died or were converted to hospice.
Our order set, “Cirrhosis Management Panel,” was created as a stand-alone order set and was embedded in the “General Admission” order set. It consisted of 8 categories, many being common complications of portal hypertension (Figure 1). Pre-selected categories included diet, paracentesis labs, and cirrhosis education. The remainder of the categories were not automatically selected and left to user discretion.
Discussion: QI efforts have been shown to standardize care between providers and across medical systems. We created an admission order set tailored towards patients with decompensated cirrhosis with the goal of optimizing evidence-based, quality care. Future work will include collecting post-intervention data to evaluate the order set’s impact on patient outcomes. We believe our order set is generalizable to other institutions and is important in encouraging conversations about how to promote QI within the cirrhosis population.
1. Wells C, et al. Standardized Hospital Order Sets in Acute Care: A Review of Clinical Evidence, Cost-Effectiveness, and Guidelines. CADTH; 2019.
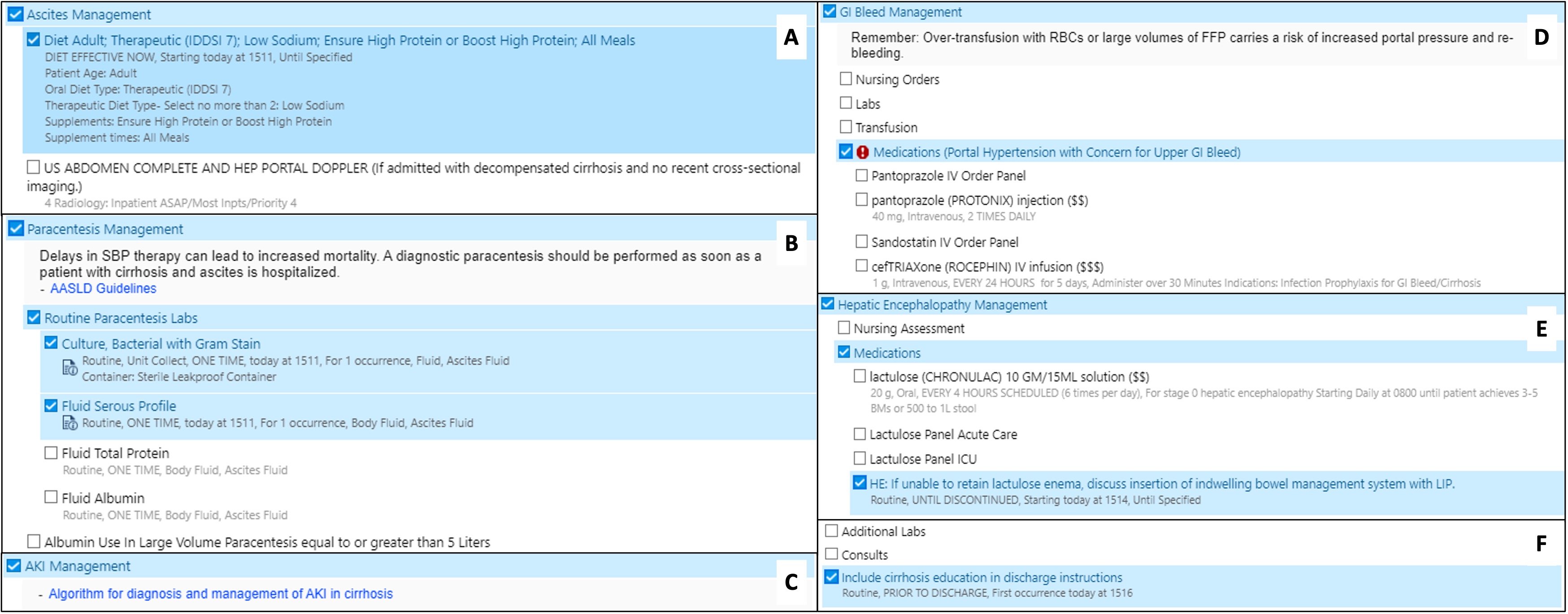
Figure: Figure 1. Cirrhosis admission order set categories including (A) Ascites Management, (B) Paracentesis Management, (C) Acute Kidney Injury (AKI) Management, (D) Gastrointestinal (GI) Bleed Management, (E) Hepatic Encephalopathy Management, (F) Labs, Consults, and Education.
Disclosures:
Laura Lavette indicated no relevant financial relationships.
Hannah Laird indicated no relevant financial relationships.
Mira Sridharan indicated no relevant financial relationships.
Jessica Dreicer indicated no relevant financial relationships.
Andrew Barros indicated no relevant financial relationships.
Kyle Enfield indicated no relevant financial relationships.
Zachary Henry indicated no relevant financial relationships.
Laura E. Lavette, MD, Hannah Laird, MD, Mira Sridharan, , Jessica Dreicer, MD, Andrew Barros, MD, Kyle Enfield, MD, Zachary Henry, MD. P4595 - Quality Improvement in Decompensated Cirrhosis: Standardizing the Admission Process, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
