Tuesday Poster Session
Category: Liver
P4704 - A Large Portal Vein Aneurysm in the Absence of Portal Hypertension Managed Conservatively With Monitoring
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SC
Susie Choi, MD
HCA Healthcare
Denver, CO
Presenting Author(s)
Susie Choi, MD1, Todd Yeates, MD2, Matthew Stotts, MD, MPH3
1HCA Healthcare, Denver, CO; 2Sky Ridge Medical Center, Lone Tree, CO; 3Presbyterian/St. Luke's Medical Center, Denver, CO
Introduction: Portal vein aneurysm (PVA) is a rare vascular abnormality for which standardized management guidelines are lacking. Herein we present a large PVA occurring in the absence of portal hypertension managed with conservative monitoring.
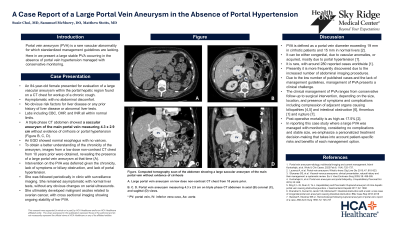
Case Description/Methods: An 84-year-old female presented for evaluation of a large vascular aneurysm within the portal hepatic region found on a CT chest for workup of a chronic cough. She was asymptomatic, denying any abdominal discomfort. She had no obvious risk factors for liver disease and was without any prior history of liver disease or abnormal liver tests. Labs including CBC, CMP, and INR were all within normal limits. A triple phase CT abdomen showed a saccular aneurysm of the main portal vein measuring 4.3 x 2.9 cm without evidence of cirrhosis or portal hypertension. An EGD showed normal esophagus with no varices. To obtain a better understanding of the chronicity of the aneurysm, images from a low dose non-contrast CT chest from 10 years prior were obtained, revealing the presence of a large portal vein aneurysm at that time.
Intervention on the PVA was deferred given the chronicity, lack of symptoms or biliary obstruction, and lack of portal hypertension. She was followed periodically in clinic and she remained asymptomatic with normal liver tests, without any obvious changes on serial ultrasounds. She ultimately developed malignant ascites related to ovarian cancer, with cross-sectional imaging showing ongoing stability of her PVA.
Discussion: PVA is defined as a portal vein diameter exceeding 19 mm in cirrhotic patients and 15 mm in normal liver. It is rare, with around 280 reported cases worldwide. It can be either congenital, due to vascular anomalies, or acquired, mostly due to portal hypertension. The clinical management of PVA ranges from conservative follow-up to surgical intervention, depending on the presence of symptoms and complications including compression of adjacent organs such as biliopathies and intestinal obstruction, thrombus and rupture. Due to the low number of published cases and the lack of management guidelines, management of PVA presents a clinical challenge. In reporting this case study where a large PVA was managed with monitoring, considering no complications and stable size, we emphasize personalized treatment decision-making that takes into account patient-specific risks and benefits of each management option.

Disclosures:
Susie Choi, MD1, Todd Yeates, MD2, Matthew Stotts, MD, MPH3. P4704 - A Large Portal Vein Aneurysm in the Absence of Portal Hypertension Managed Conservatively With Monitoring, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Healthcare, Denver, CO; 2Sky Ridge Medical Center, Lone Tree, CO; 3Presbyterian/St. Luke's Medical Center, Denver, CO
Introduction: Portal vein aneurysm (PVA) is a rare vascular abnormality for which standardized management guidelines are lacking. Herein we present a large PVA occurring in the absence of portal hypertension managed with conservative monitoring.
Case Description/Methods: An 84-year-old female presented for evaluation of a large vascular aneurysm within the portal hepatic region found on a CT chest for workup of a chronic cough. She was asymptomatic, denying any abdominal discomfort. She had no obvious risk factors for liver disease and was without any prior history of liver disease or abnormal liver tests. Labs including CBC, CMP, and INR were all within normal limits. A triple phase CT abdomen showed a saccular aneurysm of the main portal vein measuring 4.3 x 2.9 cm without evidence of cirrhosis or portal hypertension. An EGD showed normal esophagus with no varices. To obtain a better understanding of the chronicity of the aneurysm, images from a low dose non-contrast CT chest from 10 years prior were obtained, revealing the presence of a large portal vein aneurysm at that time.
Intervention on the PVA was deferred given the chronicity, lack of symptoms or biliary obstruction, and lack of portal hypertension. She was followed periodically in clinic and she remained asymptomatic with normal liver tests, without any obvious changes on serial ultrasounds. She ultimately developed malignant ascites related to ovarian cancer, with cross-sectional imaging showing ongoing stability of her PVA.
Discussion: PVA is defined as a portal vein diameter exceeding 19 mm in cirrhotic patients and 15 mm in normal liver. It is rare, with around 280 reported cases worldwide. It can be either congenital, due to vascular anomalies, or acquired, mostly due to portal hypertension. The clinical management of PVA ranges from conservative follow-up to surgical intervention, depending on the presence of symptoms and complications including compression of adjacent organs such as biliopathies and intestinal obstruction, thrombus and rupture. Due to the low number of published cases and the lack of management guidelines, management of PVA presents a clinical challenge. In reporting this case study where a large PVA was managed with monitoring, considering no complications and stable size, we emphasize personalized treatment decision-making that takes into account patient-specific risks and benefits of each management option.

Figure: CT images of portal vein aneurysm. (A) Low dose non-contrast CT chest 10 years prior. Current triple phase CT abdomen (B) axial, (C) coronal, (D) sagittal.
Disclosures:
Susie Choi indicated no relevant financial relationships.
Todd Yeates indicated no relevant financial relationships.
Matthew Stotts indicated no relevant financial relationships.
Susie Choi, MD1, Todd Yeates, MD2, Matthew Stotts, MD, MPH3. P4704 - A Large Portal Vein Aneurysm in the Absence of Portal Hypertension Managed Conservatively With Monitoring, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
