Tuesday Poster Session
Category: Practice Management
P4920 - Optimizing Efficiency in Endoscopy by Improving Room Turnover Time: A Microsystem Level Approach
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nemuel Y. Abasta
The University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Nemuel Y. Abasta, 1, Stephanie Rosser, 2, Sharon Boening, BSN, RN2
1The University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
Introduction: Demand for endoscopy continues to rise due to increasing gastrointestinal diseases. Operational efficiency is critical in meeting the capacity challenge while maintaining patient safety and maximizing return on investment (ROI). Room Turnover Time (TOT) is non-value and non-productive, negatively affecting the ROI and overall productivity. The quality improvement project (QIP) aimed to implement processes to facilitate 70% of outpatient endoscopy procedures meeting the 15-minute benchmark for room TOT at our high-volume academic tertiary care endoscopy unit over 12 weeks.
Methods: Kurt Lewin’s change theory and Lean principles guided the development of the QIP. The multidisciplinary team implemented a redesign process by creating a unit-based Process Improvement Team (PIT) Crew, which oversaw the development and implementation of the QIP. Mandatory education was provided to raise awareness of the inefficiencies of room TOT identified during value stream mapping. Visual management tools such as metrics reports via bulletins and countdown timers were used to reinforce the new process and as an accountability aid for the remaining time-lapse for TOT. Encrypted chat via electronic health record was used to improve workflow communication, and the pre-operative checklist was revised to streamline documentation and identify incomplete pre-operative activities requiring action.
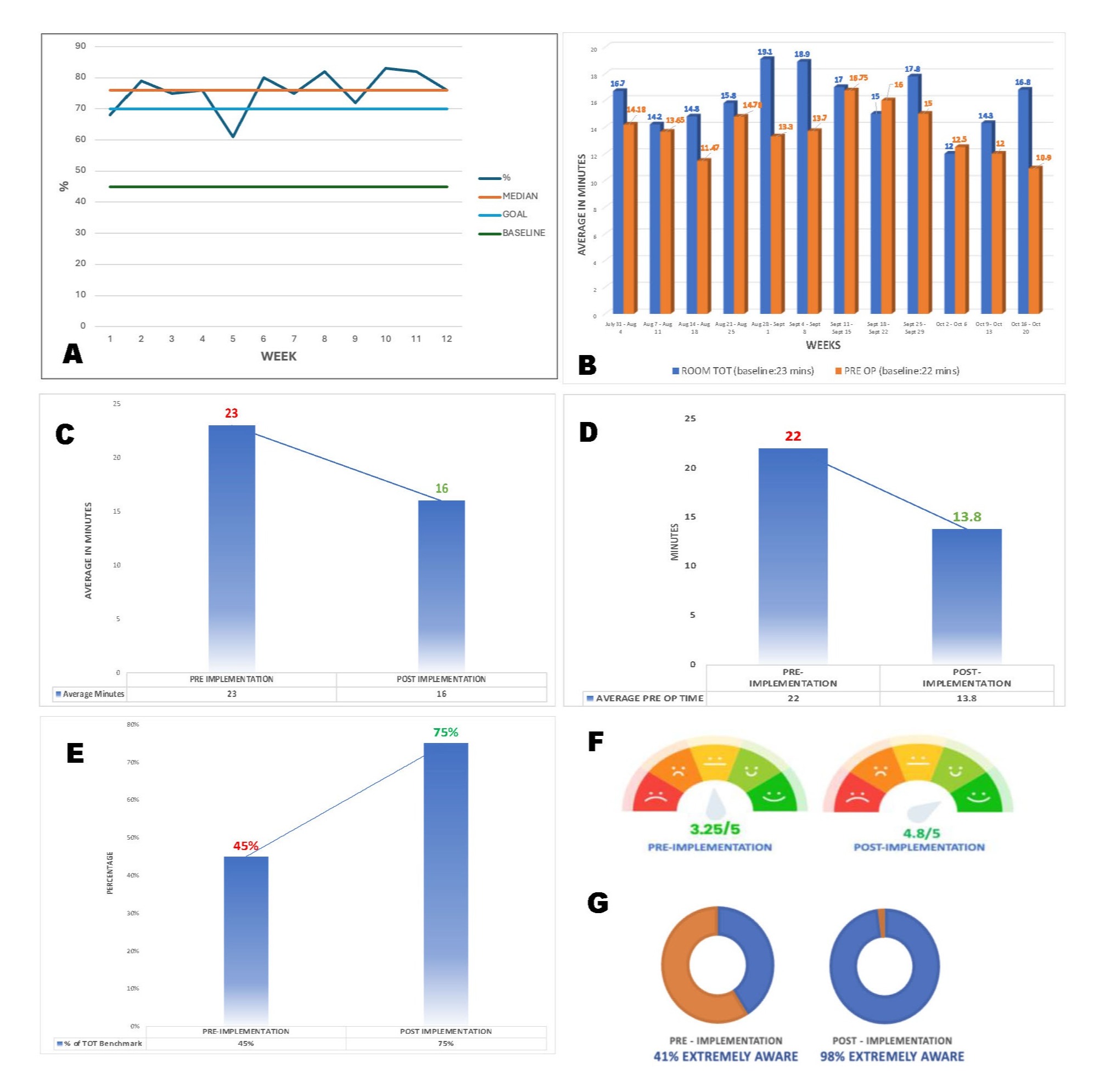
Results: Over a 12-week implementation period, 515 procedures met the inclusion criteria. Of these, 75% of the procedures met the TOT benchmark – a 67% increase from baseline (45%). Case start delays were reduced to 25% from 55%. A 30% reduction in average room TOT yielded 16 minutes, 7 minutes faster than the baseline of 23 minutes. A 98% adherence of nurses with the revamped pre-op checklist afforded a reduction of the average pre-op time from 22 minutes to 13.8 minutes (37%). Results showed a marked increase in staff satisfaction level of the redesigned process from 3.1/5 to 4.8/5 on the rating scale and performance metrics awareness level from 41% to 98%.
Discussion: The use of Lean principles effectively optimized the microsystem performance level. The results exemplified the importance of investing in human factors, the relevance of interdisciplinary collaboration, and sharing performance metrics in reducing room TOT. The marked improvement in efficiency projected over a year can add 720 outpatient procedures, which improves patient access and procedure volumes with minor costs to the department and hospital.
Disclosures:
Nemuel Y. Abasta, 1, Stephanie Rosser, 2, Sharon Boening, BSN, RN2. P4920 - Optimizing Efficiency in Endoscopy by Improving Room Turnover Time: A Microsystem Level Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
Introduction: Demand for endoscopy continues to rise due to increasing gastrointestinal diseases. Operational efficiency is critical in meeting the capacity challenge while maintaining patient safety and maximizing return on investment (ROI). Room Turnover Time (TOT) is non-value and non-productive, negatively affecting the ROI and overall productivity. The quality improvement project (QIP) aimed to implement processes to facilitate 70% of outpatient endoscopy procedures meeting the 15-minute benchmark for room TOT at our high-volume academic tertiary care endoscopy unit over 12 weeks.
Methods: Kurt Lewin’s change theory and Lean principles guided the development of the QIP. The multidisciplinary team implemented a redesign process by creating a unit-based Process Improvement Team (PIT) Crew, which oversaw the development and implementation of the QIP. Mandatory education was provided to raise awareness of the inefficiencies of room TOT identified during value stream mapping. Visual management tools such as metrics reports via bulletins and countdown timers were used to reinforce the new process and as an accountability aid for the remaining time-lapse for TOT. Encrypted chat via electronic health record was used to improve workflow communication, and the pre-operative checklist was revised to streamline documentation and identify incomplete pre-operative activities requiring action.
Results: Over a 12-week implementation period, 515 procedures met the inclusion criteria. Of these, 75% of the procedures met the TOT benchmark – a 67% increase from baseline (45%). Case start delays were reduced to 25% from 55%. A 30% reduction in average room TOT yielded 16 minutes, 7 minutes faster than the baseline of 23 minutes. A 98% adherence of nurses with the revamped pre-op checklist afforded a reduction of the average pre-op time from 22 minutes to 13.8 minutes (37%). Results showed a marked increase in staff satisfaction level of the redesigned process from 3.1/5 to 4.8/5 on the rating scale and performance metrics awareness level from 41% to 98%.
Discussion: The use of Lean principles effectively optimized the microsystem performance level. The results exemplified the importance of investing in human factors, the relevance of interdisciplinary collaboration, and sharing performance metrics in reducing room TOT. The marked improvement in efficiency projected over a year can add 720 outpatient procedures, which improves patient access and procedure volumes with minor costs to the department and hospital.
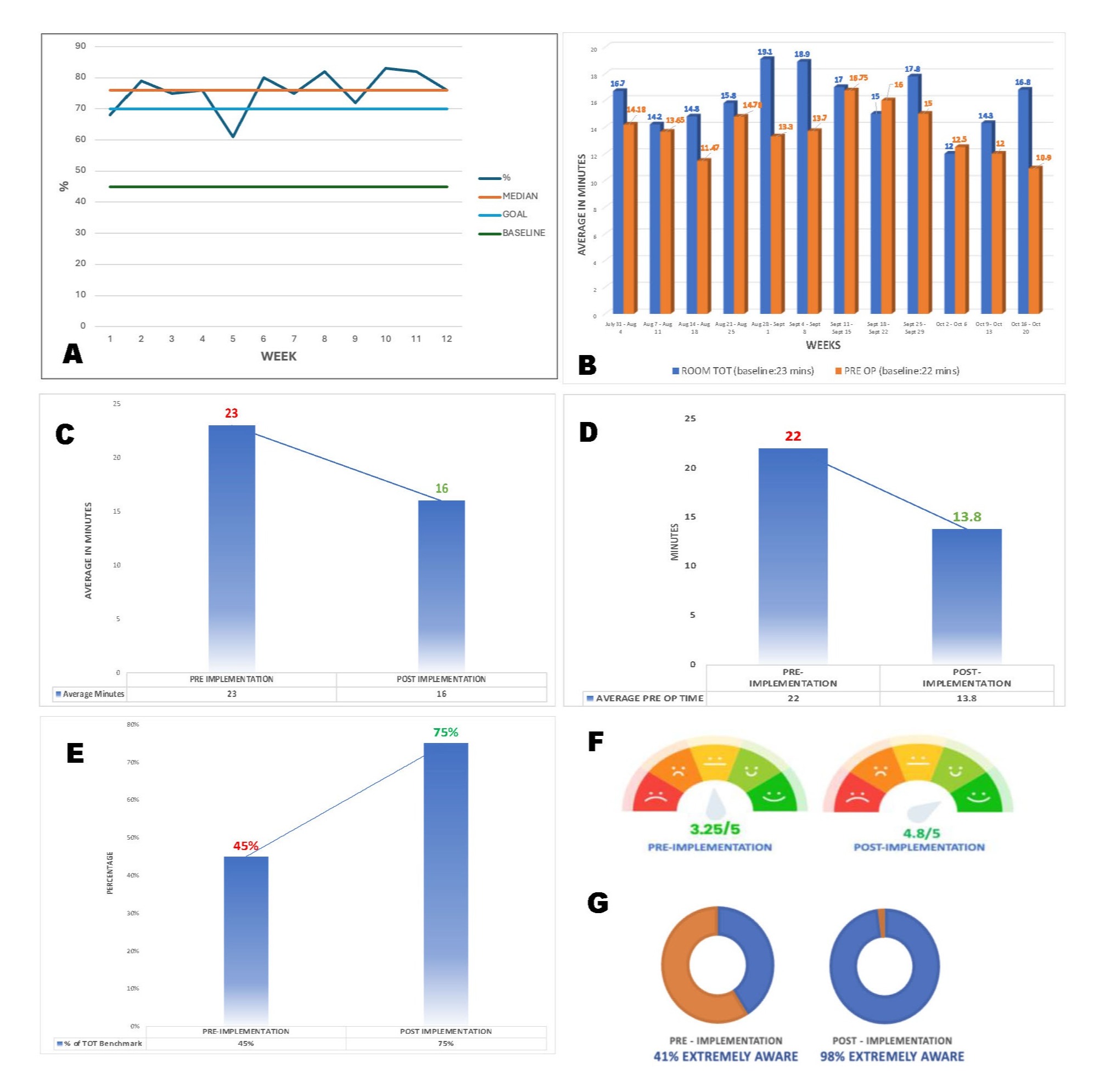
Figure: A - 12 Week Run Chart of Cases Meeting the Turnover Time Benchmark, B - Weekly Average Room Turnover Time & Pre-op Time, C - Average Room Turnover Time, D - Average Preoperative Time, E - Overall Cases Meeting the Turnover Time Benchmark, F - Staff Satisfaction Level with Redesign Workflow Process, G - Staff Awareness Level with Metrics & Benchmark
Disclosures:
Nemuel Abasta indicated no relevant financial relationships.
Stephanie Rosser indicated no relevant financial relationships.
Sharon Boening indicated no relevant financial relationships.
Nemuel Y. Abasta, 1, Stephanie Rosser, 2, Sharon Boening, BSN, RN2. P4920 - Optimizing Efficiency in Endoscopy by Improving Room Turnover Time: A Microsystem Level Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
