Tuesday Poster Session
Category: Stomach
P5134 - Acute Phlegmonous Gastritis Secondary to Oropharyngeal Group A Streptococcal Translocation via the Esophagus
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Fahad Sarvari, MD
Mercyhealth
Rockford, IL
Presenting Author(s)
Fahad Sarvari, MD1, Moamen Al Zoubi, MD1, Thayer Hamoudah, MD2, Altaf Dawood, MD, MBBS2, Naser Khan, MD2
1Mercyhealth, Rockford, IL; 2Mercy Health, Rockford, IL
Introduction: Group A streptococcal pharyngitis rarely progresses to severe illness, and if so, disseminates hematogenously to incite Toxic Shock Syndrome. Gastrointestinal inoculation may occur as a sequela of the bacteremia. Here we report a novel case of phlegmonous gastritis without bacteremia suggesting pathogen translocation from the pharynx to the stomach via the esophagus.
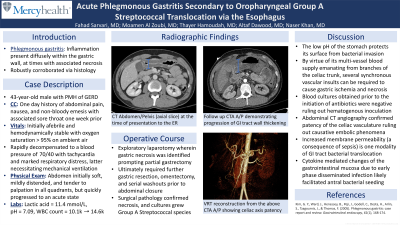
Case Description/Methods: A 43-year-old male with history of GERD presented to the emergency room with acute abdominal pain and associated sore throat, the latter ongoing for one week. Laboratory work up was noncontributory. On physical exam the abdomen was soft, tender, and mildly distended. Abdominal CTA revealed diffuse antral wall and duodenal thickening with preserved celiac axis flow thus disposition was inpatient observation with bowel rest and PPI therapy. The patient decompensated requiring intubation and pressor support in the setting of a new severe lactic acidosis (11, pH 7.09). Repeat abdominal imaging showed new thickening of the jejunum and proximal ileum thus he underwent emergent laparotomy with partial gastrectomy due to visible necrosis. Ultimately, gastric wedge resection, omentectomy, and serial abdominal washouts occurred prior to abdominal closure. Surgical culture grew group A streptococcus with negative blood cultures throughout the hospitalization suggesting a final diagnosis of phlegmonous gastritis with an alternate conduit to the stomach than the bloodstream.
Discussion: Phlegmonous gastritis involves diffuse gastric wall inflammation, at times with necrosis. The stomach is protected from most infectious and vascular causes of necrosis by its low surface pH and multivessel blood supply. Systemic inflammation facilitates gastrointestinal mucosal bacterial translocation via cytokine signaling cascade effects. In our patient, abdominal CT angiography corroborated celiac axis patency ruling out causative embolic phenomenon. Infectious work up only revealed group A streptococcus on surgical culture. Blood cultures were negative – including those drawn before antibiotic administration, all in the context of a sore throat prior to abdominal symptoms. The patient likely presented with early sepsis due to strep pharyngitis and cytokine effects facilitated antral seeding upon an inflamed gastric milieu given his history of GERD. The reports of gastric necrosis due to strep species are limited. None comment on spontaneous esophageal translocation highlighting this case as a unique presentation of a rare disease.
Disclosures:
Fahad Sarvari, MD1, Moamen Al Zoubi, MD1, Thayer Hamoudah, MD2, Altaf Dawood, MD, MBBS2, Naser Khan, MD2. P5134 - Acute Phlegmonous Gastritis Secondary to Oropharyngeal Group A Streptococcal Translocation via the Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mercyhealth, Rockford, IL; 2Mercy Health, Rockford, IL
Introduction: Group A streptococcal pharyngitis rarely progresses to severe illness, and if so, disseminates hematogenously to incite Toxic Shock Syndrome. Gastrointestinal inoculation may occur as a sequela of the bacteremia. Here we report a novel case of phlegmonous gastritis without bacteremia suggesting pathogen translocation from the pharynx to the stomach via the esophagus.
Case Description/Methods: A 43-year-old male with history of GERD presented to the emergency room with acute abdominal pain and associated sore throat, the latter ongoing for one week. Laboratory work up was noncontributory. On physical exam the abdomen was soft, tender, and mildly distended. Abdominal CTA revealed diffuse antral wall and duodenal thickening with preserved celiac axis flow thus disposition was inpatient observation with bowel rest and PPI therapy. The patient decompensated requiring intubation and pressor support in the setting of a new severe lactic acidosis (11, pH 7.09). Repeat abdominal imaging showed new thickening of the jejunum and proximal ileum thus he underwent emergent laparotomy with partial gastrectomy due to visible necrosis. Ultimately, gastric wedge resection, omentectomy, and serial abdominal washouts occurred prior to abdominal closure. Surgical culture grew group A streptococcus with negative blood cultures throughout the hospitalization suggesting a final diagnosis of phlegmonous gastritis with an alternate conduit to the stomach than the bloodstream.
Discussion: Phlegmonous gastritis involves diffuse gastric wall inflammation, at times with necrosis. The stomach is protected from most infectious and vascular causes of necrosis by its low surface pH and multivessel blood supply. Systemic inflammation facilitates gastrointestinal mucosal bacterial translocation via cytokine signaling cascade effects. In our patient, abdominal CT angiography corroborated celiac axis patency ruling out causative embolic phenomenon. Infectious work up only revealed group A streptococcus on surgical culture. Blood cultures were negative – including those drawn before antibiotic administration, all in the context of a sore throat prior to abdominal symptoms. The patient likely presented with early sepsis due to strep pharyngitis and cytokine effects facilitated antral seeding upon an inflamed gastric milieu given his history of GERD. The reports of gastric necrosis due to strep species are limited. None comment on spontaneous esophageal translocation highlighting this case as a unique presentation of a rare disease.
Disclosures:
Fahad Sarvari indicated no relevant financial relationships.
Moamen Al Zoubi indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Fahad Sarvari, MD1, Moamen Al Zoubi, MD1, Thayer Hamoudah, MD2, Altaf Dawood, MD, MBBS2, Naser Khan, MD2. P5134 - Acute Phlegmonous Gastritis Secondary to Oropharyngeal Group A Streptococcal Translocation via the Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
