Tuesday Poster Session
Category: IBD
P4343 - Toxic Megacolon Not Associated With Inflammatory Bowel Disease is Associated With Increased Mortality
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Joseph Gunderson
University of Arizona College of Medicine
Tucson, AZ
Presenting Author(s)
Joseph Gunderson, 1, David Schaub, BS1, Alisia C. Tumac, 1, Mark Borgstrom, PhD2, Sasha Taleban, MD3
1University of Arizona College of Medicine, Tucson, AZ; 2The University of Arizona, Tucson, AZ; 3University of Arizona, Tucson, AZ
Introduction: Toxic megacolon (TM) is a life-threatening condition classically linked to inflammatory bowel disease (TM-IBD) and other disease processes (TM-non-IBD). The Jalan Criteria (JC) has guided TM diagnosis since 1969, but its diagnostic sensitivity in current practice is unclear. This study aimed to identify the most common TM etiologies, compare TM disease course in IBD and non-IBD patients, and evaluate the sensitivity of the JC.
Methods: A retrospective chart review of 488 Banner Health sites from January 2014 to May 2023 identified all TM cases. Demographics, Charlson Comorbidity Index (CCI), TM etiologies, JC status, clinical and laboratory data, treatment approach, and 7- and 30-day mortality were collected. Chi-Squared, analysis of variance, and Kaplan-Meier analysis assessed differences between TM-IBD and TM-non-IBD.
Results: 106 TM cases were identified. The underlying etiology included Clostridioides difficile (43.4%), ischemic colitis (33%), ulcerative colitis (13.2%), Crohn disease (2.8%), diverticulitis (2.8%), and other (4.8%).
Mean age was 61, overall, and 51.6 and 62.7 for TM-IBD and TM-non-IBD (p < 0.01), respectively. 44.3% of all patients were female, and 70.8% were non-Hispanic white. Mean CCI was 4.4 overall, and 0.6 and 5, for TM-IBD and TM-non-IBD (p < 0.01), respectively. Among TM-non-IBD patients, 36% developed TM during their hospital course. JC sensitivity was 52.8% overall, with no significant difference for TM-IBD and TM-non-IBD.
TM-non-IBD more often presented with hemodynamic instability (67.4% vs. 41.2%, p=0.04), hypothermia (22.5% vs. 0%, p=0.03), and higher mean leukocyte (28.8 vs. 12.5 x103/μL, p < 0.01) and lactic acid (5.1 vs. 2.4 mmol/L, p=0.02) levels. TM-IBD more often presented with bloody stools (41.2% vs. 11.2%, p=0.02), and was associated with higher rates of perforation (47.1% vs. 23.6%, p < 0.05). Colectomy was performed in 59.4% of cases. Colectomy was indicated but deferred in 30.3% of TM-non-IBD cases due to poor patient surgical candidacy.
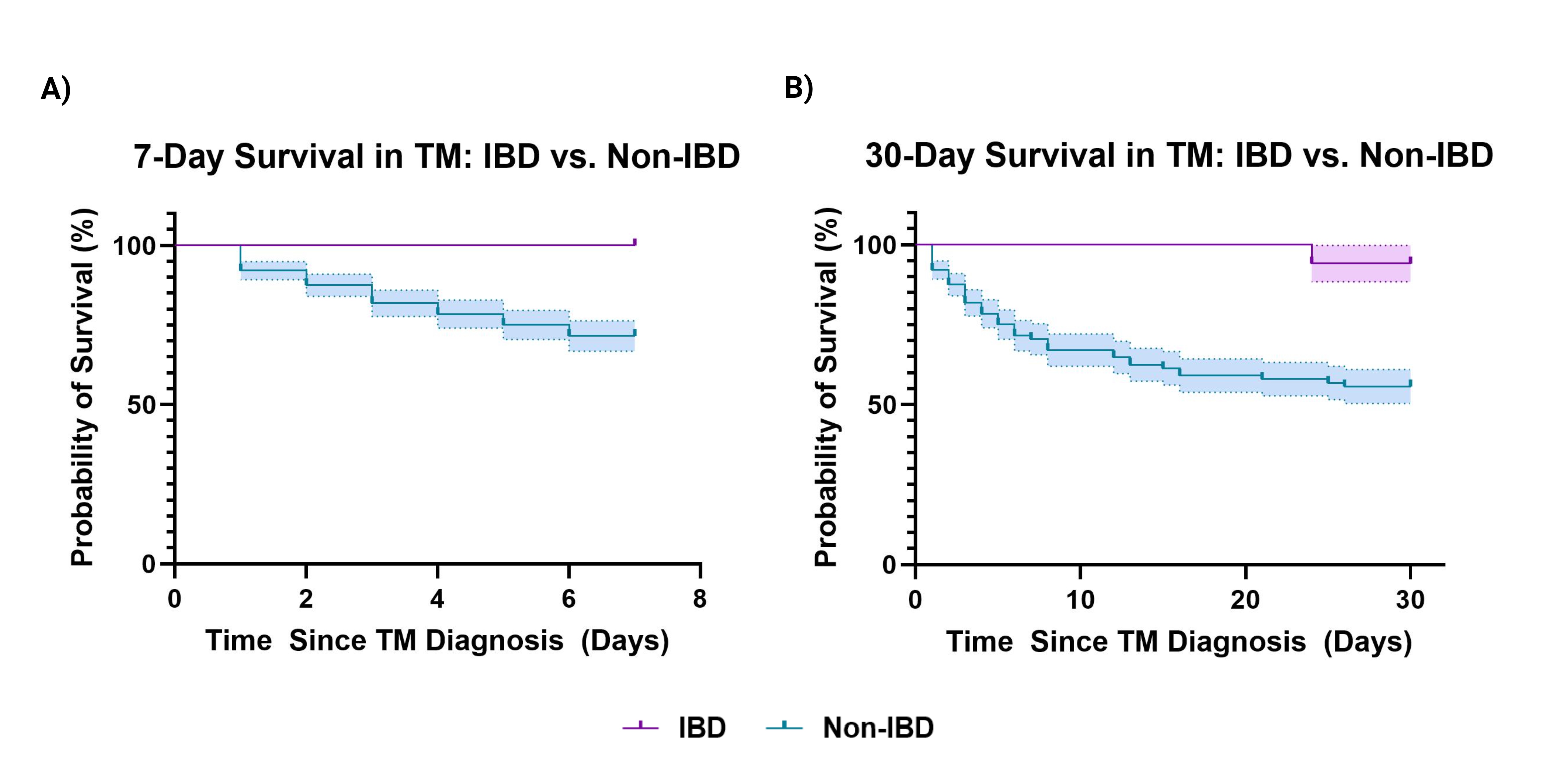
TM-non-IBD was associated with higher mortality at 7 (30.3% vs. 0%, HR 3.6, p=0.02) and 30 days (46.1% vs. 5.9%, HR 9.7, p < 0.01).
Discussion: The etiology of TM appears to have shifted toward non-IBD etiologies. Patients with TM-non-IBD are older, have a higher comorbidity index, and higher overall mortality despite lower perforation rates. Finally, the JC is poorly sensitive for TM diagnosis irrespective of the etiology.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joseph Gunderson, 1, David Schaub, BS1, Alisia C. Tumac, 1, Mark Borgstrom, PhD2, Sasha Taleban, MD3. P4343 - Toxic Megacolon Not Associated With Inflammatory Bowel Disease is Associated With Increased Mortality, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Arizona College of Medicine, Tucson, AZ; 2The University of Arizona, Tucson, AZ; 3University of Arizona, Tucson, AZ
Introduction: Toxic megacolon (TM) is a life-threatening condition classically linked to inflammatory bowel disease (TM-IBD) and other disease processes (TM-non-IBD). The Jalan Criteria (JC) has guided TM diagnosis since 1969, but its diagnostic sensitivity in current practice is unclear. This study aimed to identify the most common TM etiologies, compare TM disease course in IBD and non-IBD patients, and evaluate the sensitivity of the JC.
Methods: A retrospective chart review of 488 Banner Health sites from January 2014 to May 2023 identified all TM cases. Demographics, Charlson Comorbidity Index (CCI), TM etiologies, JC status, clinical and laboratory data, treatment approach, and 7- and 30-day mortality were collected. Chi-Squared, analysis of variance, and Kaplan-Meier analysis assessed differences between TM-IBD and TM-non-IBD.
Results: 106 TM cases were identified. The underlying etiology included Clostridioides difficile (43.4%), ischemic colitis (33%), ulcerative colitis (13.2%), Crohn disease (2.8%), diverticulitis (2.8%), and other (4.8%).
Mean age was 61, overall, and 51.6 and 62.7 for TM-IBD and TM-non-IBD (p < 0.01), respectively. 44.3% of all patients were female, and 70.8% were non-Hispanic white. Mean CCI was 4.4 overall, and 0.6 and 5, for TM-IBD and TM-non-IBD (p < 0.01), respectively. Among TM-non-IBD patients, 36% developed TM during their hospital course. JC sensitivity was 52.8% overall, with no significant difference for TM-IBD and TM-non-IBD.
TM-non-IBD more often presented with hemodynamic instability (67.4% vs. 41.2%, p=0.04), hypothermia (22.5% vs. 0%, p=0.03), and higher mean leukocyte (28.8 vs. 12.5 x103/μL, p < 0.01) and lactic acid (5.1 vs. 2.4 mmol/L, p=0.02) levels. TM-IBD more often presented with bloody stools (41.2% vs. 11.2%, p=0.02), and was associated with higher rates of perforation (47.1% vs. 23.6%, p < 0.05). Colectomy was performed in 59.4% of cases. Colectomy was indicated but deferred in 30.3% of TM-non-IBD cases due to poor patient surgical candidacy.
TM-non-IBD was associated with higher mortality at 7 (30.3% vs. 0%, HR 3.6, p=0.02) and 30 days (46.1% vs. 5.9%, HR 9.7, p < 0.01).
Discussion: The etiology of TM appears to have shifted toward non-IBD etiologies. Patients with TM-non-IBD are older, have a higher comorbidity index, and higher overall mortality despite lower perforation rates. Finally, the JC is poorly sensitive for TM diagnosis irrespective of the etiology.
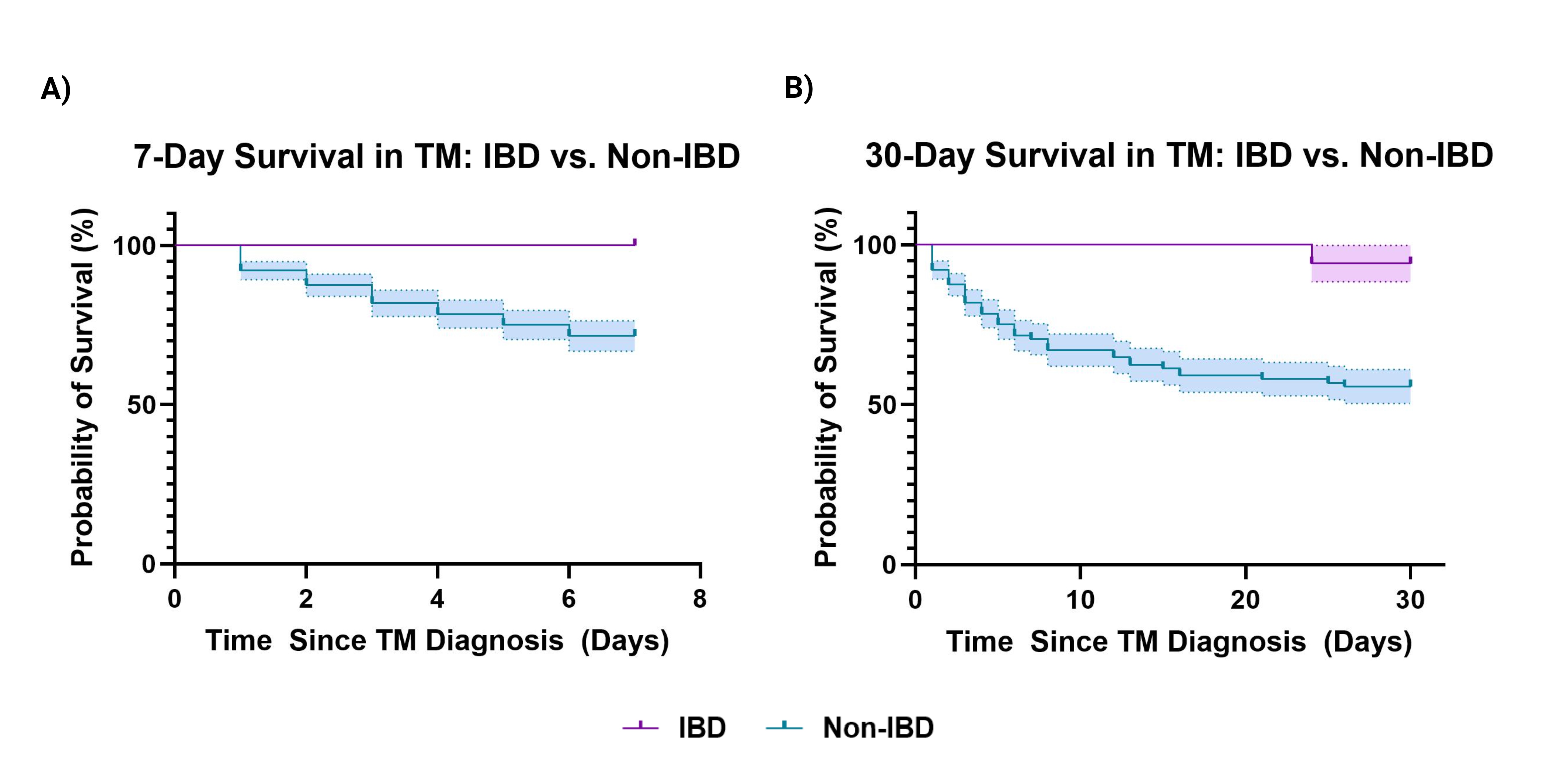
Figure: Figure 1: Kaplan-Meier survival curves comparing survival at 7 days (A) and 30 days (B) for patients with toxic megacolon associated with and without inflammatory bowel disease.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joseph Gunderson indicated no relevant financial relationships.
David Schaub indicated no relevant financial relationships.
Alisia Tumac indicated no relevant financial relationships.
Mark Borgstrom indicated no relevant financial relationships.
Sasha Taleban: AbbVie – Advisory Committee/Board Member. Bristol Myers Squibb – Grant/Research Support. Eli Lilly – Grant/Research Support. Janssen – Grant/Research Support. Pfizer – Grant/Research Support. Takeda – Grant/Research Support.
Joseph Gunderson, 1, David Schaub, BS1, Alisia C. Tumac, 1, Mark Borgstrom, PhD2, Sasha Taleban, MD3. P4343 - Toxic Megacolon Not Associated With Inflammatory Bowel Disease is Associated With Increased Mortality, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

