Tuesday Poster Session
Category: General Endoscopy
P4093 - Impact of Glucagon-Like Peptide-1 Receptor Agonist (GLP-1 RA) Use on Retained Gastric Contents and Adverse Events With Upper Endoscopy: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Syed Hamaad Rahman, DO
Methodist Dallas Medical Center
Irving, TX
Presenting Author(s)
Syed Hamaad Rahman, DO1, Nihal I. Khan, MD2, Aimen Farooq, MD3, Nouman Shafique, MD2, Mahir Qureshi, MD4, Islam Mohamed, MD5, Rami Musallam, MD6, Abu Hurairah, MD2
1Methodist Dallas Medical Center, Irving, TX; 2AdventHealth Medical Group, AdventHealth, Orlando, FL; 3AdventHealth, Orlando, FL; 4Cooper University Hospital, Philadelphia, PA; 5University of Missouri - Kansas City School of Medicine, Kansas City, MO; 6Case Western Reserve University, Cleveland, OH
Introduction: GLP-1 RAs delay gastric emptying, which may impact sedated procedures including EGDs in the form of retained gastric content (RGC) and possible aspiration events. Recently, the American Society of Anesthesiologists recommended discontinuing GLP1RAs for 1 dosing cycle prior to sedated procedures. Multiple studies have been published and presented on this topic recently, with variable results. We conducted a meta-analysis of these studies to better understand the impact of GLP1RAs.
Methods: A systematic review of the literature from MEDLINE, EMBASE and Scopus was conducted from inception to June 2024, for studies reporting on the use of GLP1RAs prior to EGDs. Outcomes of interest were RGC, aborted EGDs, adverse events (AEs), aspiration events, and need for repeat EGD. Standard meta-analysis methods were followed using the random-effects model. Heterogeneity was assessed using the I2% statistics.
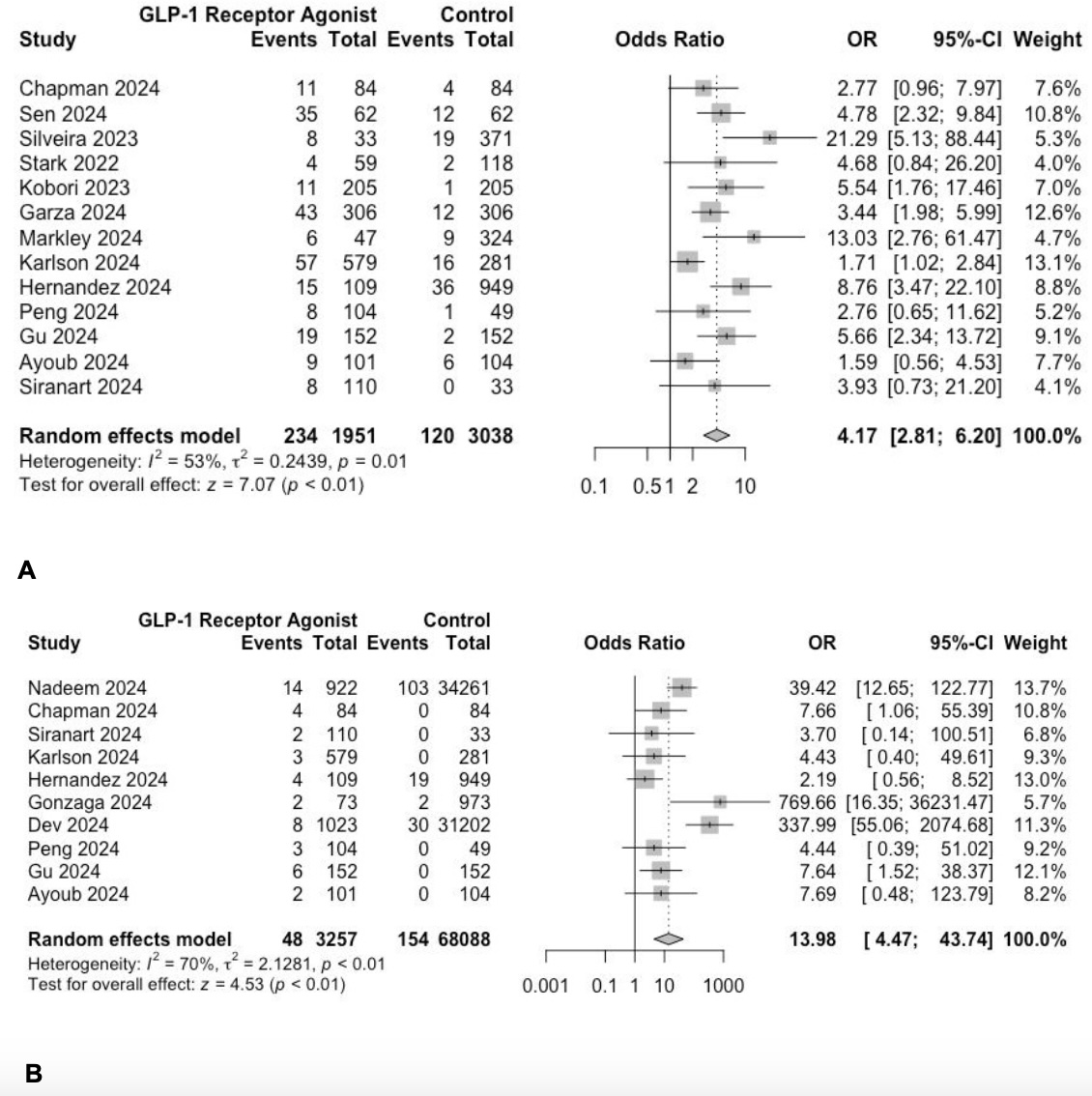
Results: 20 studies were identified, 1 study was excluded due to overlapping cohort. In the remaining 19 studies, 18 were retrospective, 1 prospective, 18 single-center, 1 multi-center, 17 case-control, and 2 single-arm studies. A total of 81,199 patients were included; 9,680 in GLP-1 RA group, and 71,519 in control group. Our results showed a statistically significant increase in RGC in patients who received GLP-1 RA (OR=4.17, 95% CI [2.81-6.2], p< 0.01, I2=53%). There was also a statistically significant increase in aborted procedures in patients who received GLP-1 RA (OR=13.98, 95% CI [4.47-43.74], p< 0.01, I2=70%). 4 studies reported on the number of AEs between groups, with 2/1359 (0.15%) patients in the GLP-1 RA group and 68/34975 (0.19%) in the control group. 8 studies compared the number of aspiration events, with 1/2589 (0.04%) in the GLP-1 RA group and 2/67625 (0.002%) in the control group.
Discussion: Our meta-analysis of 19 studies revealed a statistically significant increase in RGC and aborted procedures in the GLP-1 RA group. However, there was a negligible number of AEs and specifically aspiration events (< 1%) in both groups. These findings suggest that while GLP-1 RA use prior to endoscopy may result in increased rates of RGC and aborted procedures, it may not result in an increased incidence of aspiration events. A potential confounder could be the increased incidence of aborted procedures in the GLP-1 RA group, which would prevent potential AEs such as aspiration. Further studies in the form of prospective, large sample, blinded studies are needed to confirm our findings.
Disclosures:
Syed Hamaad Rahman, DO1, Nihal I. Khan, MD2, Aimen Farooq, MD3, Nouman Shafique, MD2, Mahir Qureshi, MD4, Islam Mohamed, MD5, Rami Musallam, MD6, Abu Hurairah, MD2. P4093 - Impact of Glucagon-Like Peptide-1 Receptor Agonist (GLP-1 RA) Use on Retained Gastric Contents and Adverse Events With Upper Endoscopy: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Methodist Dallas Medical Center, Irving, TX; 2AdventHealth Medical Group, AdventHealth, Orlando, FL; 3AdventHealth, Orlando, FL; 4Cooper University Hospital, Philadelphia, PA; 5University of Missouri - Kansas City School of Medicine, Kansas City, MO; 6Case Western Reserve University, Cleveland, OH
Introduction: GLP-1 RAs delay gastric emptying, which may impact sedated procedures including EGDs in the form of retained gastric content (RGC) and possible aspiration events. Recently, the American Society of Anesthesiologists recommended discontinuing GLP1RAs for 1 dosing cycle prior to sedated procedures. Multiple studies have been published and presented on this topic recently, with variable results. We conducted a meta-analysis of these studies to better understand the impact of GLP1RAs.
Methods: A systematic review of the literature from MEDLINE, EMBASE and Scopus was conducted from inception to June 2024, for studies reporting on the use of GLP1RAs prior to EGDs. Outcomes of interest were RGC, aborted EGDs, adverse events (AEs), aspiration events, and need for repeat EGD. Standard meta-analysis methods were followed using the random-effects model. Heterogeneity was assessed using the I2% statistics.
Results: 20 studies were identified, 1 study was excluded due to overlapping cohort. In the remaining 19 studies, 18 were retrospective, 1 prospective, 18 single-center, 1 multi-center, 17 case-control, and 2 single-arm studies. A total of 81,199 patients were included; 9,680 in GLP-1 RA group, and 71,519 in control group. Our results showed a statistically significant increase in RGC in patients who received GLP-1 RA (OR=4.17, 95% CI [2.81-6.2], p< 0.01, I2=53%). There was also a statistically significant increase in aborted procedures in patients who received GLP-1 RA (OR=13.98, 95% CI [4.47-43.74], p< 0.01, I2=70%). 4 studies reported on the number of AEs between groups, with 2/1359 (0.15%) patients in the GLP-1 RA group and 68/34975 (0.19%) in the control group. 8 studies compared the number of aspiration events, with 1/2589 (0.04%) in the GLP-1 RA group and 2/67625 (0.002%) in the control group.
Discussion: Our meta-analysis of 19 studies revealed a statistically significant increase in RGC and aborted procedures in the GLP-1 RA group. However, there was a negligible number of AEs and specifically aspiration events (< 1%) in both groups. These findings suggest that while GLP-1 RA use prior to endoscopy may result in increased rates of RGC and aborted procedures, it may not result in an increased incidence of aspiration events. A potential confounder could be the increased incidence of aborted procedures in the GLP-1 RA group, which would prevent potential AEs such as aspiration. Further studies in the form of prospective, large sample, blinded studies are needed to confirm our findings.
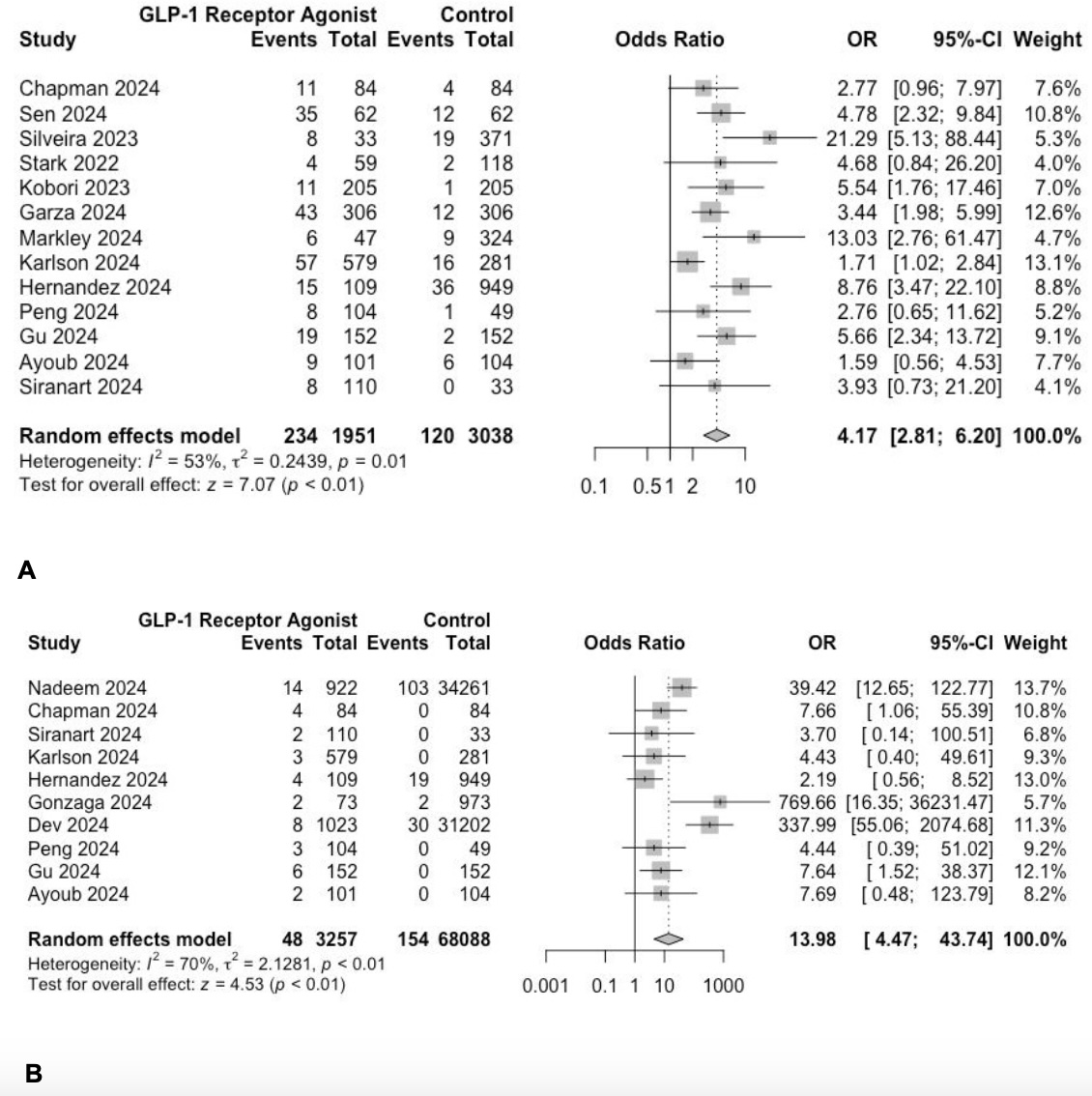
Figure: A: Forrest plot showing OR for RGC between both groups.
B: Forrest plot showing OR for aborted procedures between both groups
B: Forrest plot showing OR for aborted procedures between both groups
Disclosures:
Syed Hamaad Rahman indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Aimen Farooq indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Mahir Qureshi indicated no relevant financial relationships.
Islam Mohamed indicated no relevant financial relationships.
Rami Musallam indicated no relevant financial relationships.
Abu Hurairah indicated no relevant financial relationships.
Syed Hamaad Rahman, DO1, Nihal I. Khan, MD2, Aimen Farooq, MD3, Nouman Shafique, MD2, Mahir Qureshi, MD4, Islam Mohamed, MD5, Rami Musallam, MD6, Abu Hurairah, MD2. P4093 - Impact of Glucagon-Like Peptide-1 Receptor Agonist (GLP-1 RA) Use on Retained Gastric Contents and Adverse Events With Upper Endoscopy: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
