Tuesday Poster Session
Category: Functional Bowel Disease
P4063 - Prevalence of Bile Acid Malabsorption in IBS-D Patients: Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- PY
Pradeep Yarra, MD
Saint Louis University School of Medicine
St. Louis, MO
Presenting Author(s)
Pradeep Yarra, MD1, Shravya Ginnaram, MD2, Satyapriya Paritala, MD3, Alexander J. Thomas, MD4, Kishore Karri, MBBS, MD5, Adam D. Farmer, MD, PhD4
1Saint Louis University School of Medicine, St. Louis, MO; 2Jefferson Abington Hospital, Willow Grove, PA; 3Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 4SSM Health Saint Louis University Hospital, St. Louis, MO; 5University of Kentucky, Lexington, KY
Introduction: Irritable bowel syndrome with diarrhea (IBS-D), characterized by abdominal pain and watery diarrhea, has a global prevalence rate of up to 10%. Bile acid diarrhea (BAD) is present in 25% to 50% of IBS-D patients, compared to approximately 1% of the general population, however its impact is not well understood. This study aims to elucidate the prevalence of BAD among IBS-D patients.
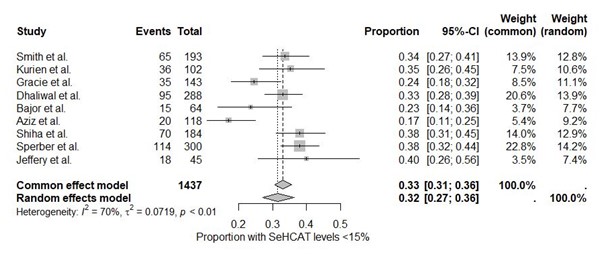
Methods: A systematic review and meta-analysis were conducted based on PRISMA guidelines. MEDLINE/Pubmed, Scopus and OVID databases were searched up from inception to May 2024. Nine studies recruiting adults with IBS-D, defined by the Manning, Kruis, Rome I, II, III or IV criteria and which used (SeHCAT) testing for the assessment of BAD were included. The primary outcome was the proportion of IBS-D patients with SeHCAT retention levels of less than 15%, indicating malabsorption/BAD.
Results: The combined analysis included 1,437 IBS-D patients. The proportion of patients with SeHCAT levels < 15% was calculated using a random-effects model due to significant heterogeneity (I² = 70%, τ² = 0.0719, p < 0.01). The random-effects model estimated that 32% (95% CI: 27% to 36%) of IBS-D patients had SeHCAT retention levels < 15%.
Discussion: The study revealed that approximately one-third of IBS-D patients exhibit BAD as indicated by SeHCAT retention levels < 15%. This considerable proportion highlights the importance of considering BAD in the differential diagnosis and management of IBS-D. The 23-seleno-25-homotaurocholic acid (SeHCAT) test, crucial for diagnosing BAD, is unavailable in the USA, necessitating alternatives like serum C4, FGF19 assessments, or fecal bile acid measurements. Future research should focus on standardizing diagnostic criteria for BAD and exploring the underlying mechanisms linking BAD with IBS-D. Longitudinal studies assessing the long-term benefits of targeted treatments for BAD in IBS-D patients would further validate the clinical importance of these findings.
Disclosures:
Pradeep Yarra, MD1, Shravya Ginnaram, MD2, Satyapriya Paritala, MD3, Alexander J. Thomas, MD4, Kishore Karri, MBBS, MD5, Adam D. Farmer, MD, PhD4. P4063 - Prevalence of Bile Acid Malabsorption in IBS-D Patients: Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Louis University School of Medicine, St. Louis, MO; 2Jefferson Abington Hospital, Willow Grove, PA; 3Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 4SSM Health Saint Louis University Hospital, St. Louis, MO; 5University of Kentucky, Lexington, KY
Introduction: Irritable bowel syndrome with diarrhea (IBS-D), characterized by abdominal pain and watery diarrhea, has a global prevalence rate of up to 10%. Bile acid diarrhea (BAD) is present in 25% to 50% of IBS-D patients, compared to approximately 1% of the general population, however its impact is not well understood. This study aims to elucidate the prevalence of BAD among IBS-D patients.
Methods: A systematic review and meta-analysis were conducted based on PRISMA guidelines. MEDLINE/Pubmed, Scopus and OVID databases were searched up from inception to May 2024. Nine studies recruiting adults with IBS-D, defined by the Manning, Kruis, Rome I, II, III or IV criteria and which used (SeHCAT) testing for the assessment of BAD were included. The primary outcome was the proportion of IBS-D patients with SeHCAT retention levels of less than 15%, indicating malabsorption/BAD.
Results: The combined analysis included 1,437 IBS-D patients. The proportion of patients with SeHCAT levels < 15% was calculated using a random-effects model due to significant heterogeneity (I² = 70%, τ² = 0.0719, p < 0.01). The random-effects model estimated that 32% (95% CI: 27% to 36%) of IBS-D patients had SeHCAT retention levels < 15%.
Discussion: The study revealed that approximately one-third of IBS-D patients exhibit BAD as indicated by SeHCAT retention levels < 15%. This considerable proportion highlights the importance of considering BAD in the differential diagnosis and management of IBS-D. The 23-seleno-25-homotaurocholic acid (SeHCAT) test, crucial for diagnosing BAD, is unavailable in the USA, necessitating alternatives like serum C4, FGF19 assessments, or fecal bile acid measurements. Future research should focus on standardizing diagnostic criteria for BAD and exploring the underlying mechanisms linking BAD with IBS-D. Longitudinal studies assessing the long-term benefits of targeted treatments for BAD in IBS-D patients would further validate the clinical importance of these findings.
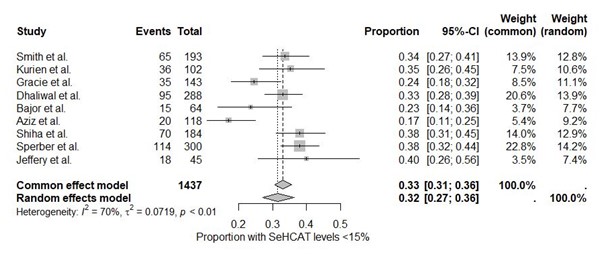
Figure: Forest Plot
Disclosures:
Pradeep Yarra indicated no relevant financial relationships.
Shravya Ginnaram indicated no relevant financial relationships.
Satyapriya Paritala indicated no relevant financial relationships.
Alexander Thomas indicated no relevant financial relationships.
Kishore Karri indicated no relevant financial relationships.
Adam Farmer indicated no relevant financial relationships.
Pradeep Yarra, MD1, Shravya Ginnaram, MD2, Satyapriya Paritala, MD3, Alexander J. Thomas, MD4, Kishore Karri, MBBS, MD5, Adam D. Farmer, MD, PhD4. P4063 - Prevalence of Bile Acid Malabsorption in IBS-D Patients: Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
