Tuesday Poster Session
Category: Biliary/Pancreas
P3547 - Pictures Aren't Always Worth a Thousand Words: Acute Cholecystitis Amidst Equivocal Imaging Studies
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- GC
Gregory M. Connors, BS (he/him/his)
Drexel University College of Medicine
Philadelphia, PA
Presenting Author(s)
Matthew E. Kent, BS, Gregory M. Connors, BS, Karen Avgush, MD
Drexel University College of Medicine, Philadelphia, PA
Introduction: The diagnosis of acute cholecystitis relies on clinical presentation, laboratory testing, and imaging. However, approximately 19% of cases present with negative or equivocal imaging findings. Hence, undue dependence on diagnostic imaging may lead to missed or delayed diagnosis.
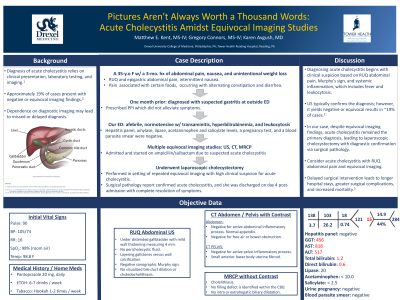
Case Description/Methods: A 35-year-old woman presented to the emergency department (ED) with a 3-month history of right upper quadrant (RUQ) and epigastric abdominal pain, intermittent nausea, and unintentional weight loss. The pain was occasionally associated with certain foods and occurred alongside alternating constipation and diarrhea.
One month earlier, she was prescribed a proton-pump inhibitor for suspected gastritis, which did not alleviate her symptoms, prompting her ED visit. In the ED she was afebrile and normotensive; however, laboratory studies revealed transaminitis, hyperbilirubinemia, and leukocytosis. Additional testing including a hepatitis panel, amylase, lipase, acetaminophen and salicylate levels, a pregnancy test, and a blood parasite smear were unrevealing.
Ultrasound (US) identified mild gallbladder wall thickening with gallstones versus calcifications. Subsequent CT scan of the abdomen and pelvis also yielded inconclusive results. Consequently, she was admitted and started on ampicillin/sulbactam due to suspected acute cholecystitis.
A magnetic resonance cholangiopancreatography (MRCP) was performed, but was inconclusive. In the setting of repeated equivocal imaging with a high clinical suspicion for acute cholecystitis, the general surgery service proceeded with laparoscopic cholecystectomy. The surgical pathology report ultimately confirmed acute cholecystitis, and she was discharged on day 4 post-admission with complete resolution of symptoms.
Discussion: Diagnosing acute cholecystitis begins with clinical suspicion based on RUQ abdominal pain, Murphy's sign, and systemic inflammation, which includes fever and leukocytosis. While US typically confirms the diagnosis, it yields negative or equivocal results in ~19% of cases. In our case, despite equivocal imaging findings, acute cholecystitis remained the primary diagnosis, ultimately leading to laparoscopic cholecystectomy with diagnostic confirmation via surgical pathology. In summary, it is crucial for physicians to consider acute cholecystitis in those presenting with RUQ abdominal pain and equivocal imaging, as delayed surgical intervention can lead to longer hospital stays, greater surgical complications, and increased mortality.
Disclosures:
Matthew E. Kent, BS, Gregory M. Connors, BS, Karen Avgush, MD. P3547 - Pictures Aren't Always Worth a Thousand Words: Acute Cholecystitis Amidst Equivocal Imaging Studies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Drexel University College of Medicine, Philadelphia, PA
Introduction: The diagnosis of acute cholecystitis relies on clinical presentation, laboratory testing, and imaging. However, approximately 19% of cases present with negative or equivocal imaging findings. Hence, undue dependence on diagnostic imaging may lead to missed or delayed diagnosis.
Case Description/Methods: A 35-year-old woman presented to the emergency department (ED) with a 3-month history of right upper quadrant (RUQ) and epigastric abdominal pain, intermittent nausea, and unintentional weight loss. The pain was occasionally associated with certain foods and occurred alongside alternating constipation and diarrhea.
One month earlier, she was prescribed a proton-pump inhibitor for suspected gastritis, which did not alleviate her symptoms, prompting her ED visit. In the ED she was afebrile and normotensive; however, laboratory studies revealed transaminitis, hyperbilirubinemia, and leukocytosis. Additional testing including a hepatitis panel, amylase, lipase, acetaminophen and salicylate levels, a pregnancy test, and a blood parasite smear were unrevealing.
Ultrasound (US) identified mild gallbladder wall thickening with gallstones versus calcifications. Subsequent CT scan of the abdomen and pelvis also yielded inconclusive results. Consequently, she was admitted and started on ampicillin/sulbactam due to suspected acute cholecystitis.
A magnetic resonance cholangiopancreatography (MRCP) was performed, but was inconclusive. In the setting of repeated equivocal imaging with a high clinical suspicion for acute cholecystitis, the general surgery service proceeded with laparoscopic cholecystectomy. The surgical pathology report ultimately confirmed acute cholecystitis, and she was discharged on day 4 post-admission with complete resolution of symptoms.
Discussion: Diagnosing acute cholecystitis begins with clinical suspicion based on RUQ abdominal pain, Murphy's sign, and systemic inflammation, which includes fever and leukocytosis. While US typically confirms the diagnosis, it yields negative or equivocal results in ~19% of cases. In our case, despite equivocal imaging findings, acute cholecystitis remained the primary diagnosis, ultimately leading to laparoscopic cholecystectomy with diagnostic confirmation via surgical pathology. In summary, it is crucial for physicians to consider acute cholecystitis in those presenting with RUQ abdominal pain and equivocal imaging, as delayed surgical intervention can lead to longer hospital stays, greater surgical complications, and increased mortality.
Disclosures:
Matthew Kent indicated no relevant financial relationships.
Gregory Connors indicated no relevant financial relationships.
Karen Avgush indicated no relevant financial relationships.
Matthew E. Kent, BS, Gregory M. Connors, BS, Karen Avgush, MD. P3547 - Pictures Aren't Always Worth a Thousand Words: Acute Cholecystitis Amidst Equivocal Imaging Studies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
