Tuesday Poster Session
Category: Colon
P3674 - Isolated Colonic Polypoid Ganglioneuromas in Patient With Neurofibromatosis Type 1
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Spandana Alluri, MS, MD
Henry Ford Health
West Bloomfield, MI
Presenting Author(s)
Spandana Alluri, MS, MD1, Tasnia Matin, MD2
1Henry Ford Health, West Bloomfield, MI; 2Henry Ford Health, Detroit, MI
Introduction: Ganglioneuromas are rare, benign neurogenic tumors arising from the peripheral nervous system, which can occur in the mediastinum, retroperitoneum, adrenal gland, and uncommonly, the GI tract. Intestinal ganglioneuromas are typically diagnosed in adolescents and young adults and can manifest as polypoid, multifocal, or diffuse involvement of the intestinal tract. While patients are often asymptomatic, large lesions can cause significant downstream effects such as Gastrointestinal bleeding, motility issues and obstruction, making recognition imperative . Diffuse ganglioneuromatosis has been associated with syndromic conditions such as MEN2B and Cowden, however association with Neurofibromatosis 1 (NF1) remains largely undocumented.
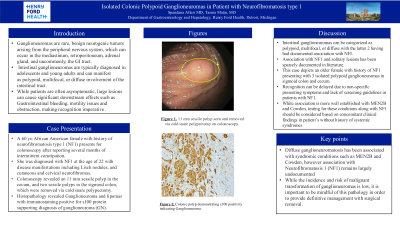
Case Description/Methods: We report the case of a 60 yo African American female with history of neurofibromatosis type 1 (NF1), who presents for colonoscopy after reporting several months of intermittent constipation. She was diagnosed with NF1 at the age of 22 with disease manifestations including Lisch nodules, and cutaneous and cervical neurofibromas. Colonoscopy unexpectedly revealed an 11 mm sessile polyp in the cecum, and two sessile polyps in the sigmoid colon, which were removed via cold snare polypectomy. Histopathology revealed Ganglioneuroma and lipomas with immunostaining positive for s100 protein supporting diagnosis of ganglioneuroma (GN).
Discussion: Intestinal ganglioneuromas can be categorized as polypoid, multifocal, or diffuse with the latter 2 having had documented association with NFI. However, association with NF1 and solitary lesions has been sparsely documented in literature. In our peculiar case, an older female with history of NF1 presented with 3 isolated polypoid ganglioneuromas in sigmoid colon and cecum. While the incidence and risk of malignant transformation of ganglioneuromas is low, it is important to be mindful of this pathology in order to provide definitive management with surgical removal. Recognition can be delayed due to non-specific presenting symptoms and lack of screening guidelines in patients with NF1. While association is more well established with MEN2B and Cowden, testing for these conditions along with NF1 should be considered based on concomitant clinical findings in patient’s without history of systemic syndromes.
Disclosures:
Spandana Alluri, MS, MD1, Tasnia Matin, MD2. P3674 - Isolated Colonic Polypoid Ganglioneuromas in Patient With Neurofibromatosis Type 1, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, West Bloomfield, MI; 2Henry Ford Health, Detroit, MI
Introduction: Ganglioneuromas are rare, benign neurogenic tumors arising from the peripheral nervous system, which can occur in the mediastinum, retroperitoneum, adrenal gland, and uncommonly, the GI tract. Intestinal ganglioneuromas are typically diagnosed in adolescents and young adults and can manifest as polypoid, multifocal, or diffuse involvement of the intestinal tract. While patients are often asymptomatic, large lesions can cause significant downstream effects such as Gastrointestinal bleeding, motility issues and obstruction, making recognition imperative . Diffuse ganglioneuromatosis has been associated with syndromic conditions such as MEN2B and Cowden, however association with Neurofibromatosis 1 (NF1) remains largely undocumented.
Case Description/Methods: We report the case of a 60 yo African American female with history of neurofibromatosis type 1 (NF1), who presents for colonoscopy after reporting several months of intermittent constipation. She was diagnosed with NF1 at the age of 22 with disease manifestations including Lisch nodules, and cutaneous and cervical neurofibromas. Colonoscopy unexpectedly revealed an 11 mm sessile polyp in the cecum, and two sessile polyps in the sigmoid colon, which were removed via cold snare polypectomy. Histopathology revealed Ganglioneuroma and lipomas with immunostaining positive for s100 protein supporting diagnosis of ganglioneuroma (GN).
Discussion: Intestinal ganglioneuromas can be categorized as polypoid, multifocal, or diffuse with the latter 2 having had documented association with NFI. However, association with NF1 and solitary lesions has been sparsely documented in literature. In our peculiar case, an older female with history of NF1 presented with 3 isolated polypoid ganglioneuromas in sigmoid colon and cecum. While the incidence and risk of malignant transformation of ganglioneuromas is low, it is important to be mindful of this pathology in order to provide definitive management with surgical removal. Recognition can be delayed due to non-specific presenting symptoms and lack of screening guidelines in patients with NF1. While association is more well established with MEN2B and Cowden, testing for these conditions along with NF1 should be considered based on concomitant clinical findings in patient’s without history of systemic syndromes.
Disclosures:
Spandana Alluri indicated no relevant financial relationships.
Tasnia Matin indicated no relevant financial relationships.
Spandana Alluri, MS, MD1, Tasnia Matin, MD2. P3674 - Isolated Colonic Polypoid Ganglioneuromas in Patient With Neurofibromatosis Type 1, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
