Sunday Poster Session
Category: Esophagus
P0544 - Unveiling the Cause of GI Symptoms in a Patient With Mpox and HIV/AIDS
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- LK
Lu-Yi Kang, DO
Kirk Kerkorian School of Medicine at the University of Nevada
Las Vegas, NV
Presenting Author(s)
Lu-Yi Kang, DO1, Chun-Han Lo, MD, MPH1, Amol Koldhekar, MD1, Rajan Amin, MD1, Vignan Manne, MD2
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV; 2Kirk Kirkorian School of Medicine, Las Vegas, NV
Introduction: Gastrointestinal symptoms are common in patients with Mpox. The etiology is often multifactorial as these patients frequently have concurrent systemic diseases. We describe a patient with monkeypox and concurrent HIV/AIDS who presented with odynophagia and nausea, later confirmed to have laryngeal involvement of Mpox, esophageal and oropharyngeal candidiasis, and CMV gastritis.
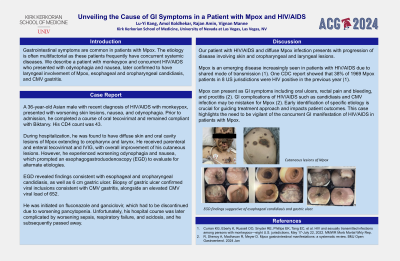
Case Description/Methods: A 36-year-old Asian male with recent diagnosis of HIV/AIDS with monkeypox, presented with worsening skin lesions, nausea, and odynophagia. Prior to admission, he completed a course of oral tecovirimat and remained compliant with Biktarvy. His CD4 count was 43. During hospitalization, he was found to have diffuse skin and oral cavity lesions of Mpox extending to oropharynx and larynx. He received parenteral and enteral tecovirimat and IVIG, with overall improvement of his cutaneous lesions. However, he experienced worsening odynophagia and nausea, which prompted an esophagogastroduodenoscopy (EGD) to evaluate for alternate etiologies. EGD revealed findings consistent with esophageal and oropharyngeal candidiasis, as well as 6 cm gastric ulcer. Biopsy of gastric ulcer confirmed viral inclusions consistent with CMV gastritis, alongside an elevated CMV viral load of 652. He was initiated on fluconazole and ganciclovir, which had to be discontinued due to worsening pancytopenia. Unfortunately, his hospital course was later complicated by worsening sepsis, respiratory failure, and acidosis, and he subsequently passed away.
Discussion: Our patient with HIV/AIDS and diffuse Mpox infection presents with progression of disease involving skin and oropharyngeal and laryngeal lesions. Mpox is an emerging disease increasingly seen in patients with HIV/AIDS due to shared mode of transmission. One CDC report showed that 38% of 1969 Mpox patients in 8 US jurisdictions were HIV positive in the previous year. Mpox can present as GI symptoms including oral ulcers, rectal pain and bleeding, and proctitis. GI complications of HIV/AIDS such as candidiasis and CMV infection may be mistaken for Mpox. Early identification of specific etiology is crucial for guiding treatment approach and impacts patient outcomes. This case highlights the need to be vigilant of the concurrent GI manifestation of HIV/AIDS in patients with Mpox.

Disclosures:
Lu-Yi Kang, DO1, Chun-Han Lo, MD, MPH1, Amol Koldhekar, MD1, Rajan Amin, MD1, Vignan Manne, MD2. P0544 - Unveiling the Cause of GI Symptoms in a Patient With Mpox and HIV/AIDS, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV; 2Kirk Kirkorian School of Medicine, Las Vegas, NV
Introduction: Gastrointestinal symptoms are common in patients with Mpox. The etiology is often multifactorial as these patients frequently have concurrent systemic diseases. We describe a patient with monkeypox and concurrent HIV/AIDS who presented with odynophagia and nausea, later confirmed to have laryngeal involvement of Mpox, esophageal and oropharyngeal candidiasis, and CMV gastritis.
Case Description/Methods: A 36-year-old Asian male with recent diagnosis of HIV/AIDS with monkeypox, presented with worsening skin lesions, nausea, and odynophagia. Prior to admission, he completed a course of oral tecovirimat and remained compliant with Biktarvy. His CD4 count was 43. During hospitalization, he was found to have diffuse skin and oral cavity lesions of Mpox extending to oropharynx and larynx. He received parenteral and enteral tecovirimat and IVIG, with overall improvement of his cutaneous lesions. However, he experienced worsening odynophagia and nausea, which prompted an esophagogastroduodenoscopy (EGD) to evaluate for alternate etiologies. EGD revealed findings consistent with esophageal and oropharyngeal candidiasis, as well as 6 cm gastric ulcer. Biopsy of gastric ulcer confirmed viral inclusions consistent with CMV gastritis, alongside an elevated CMV viral load of 652. He was initiated on fluconazole and ganciclovir, which had to be discontinued due to worsening pancytopenia. Unfortunately, his hospital course was later complicated by worsening sepsis, respiratory failure, and acidosis, and he subsequently passed away.
Discussion: Our patient with HIV/AIDS and diffuse Mpox infection presents with progression of disease involving skin and oropharyngeal and laryngeal lesions. Mpox is an emerging disease increasingly seen in patients with HIV/AIDS due to shared mode of transmission. One CDC report showed that 38% of 1969 Mpox patients in 8 US jurisdictions were HIV positive in the previous year. Mpox can present as GI symptoms including oral ulcers, rectal pain and bleeding, and proctitis. GI complications of HIV/AIDS such as candidiasis and CMV infection may be mistaken for Mpox. Early identification of specific etiology is crucial for guiding treatment approach and impacts patient outcomes. This case highlights the need to be vigilant of the concurrent GI manifestation of HIV/AIDS in patients with Mpox.

Figure: Cutaneous lesions of Mpox (top). EGD findings suggestive of esophageal candidiasis and gastric ulcer (bottom).
Disclosures:
Lu-Yi Kang indicated no relevant financial relationships.
Chun-Han Lo indicated no relevant financial relationships.
Amol Koldhekar indicated no relevant financial relationships.
Rajan Amin indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Lu-Yi Kang, DO1, Chun-Han Lo, MD, MPH1, Amol Koldhekar, MD1, Rajan Amin, MD1, Vignan Manne, MD2. P0544 - Unveiling the Cause of GI Symptoms in a Patient With Mpox and HIV/AIDS, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
